Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 1
439 - Interest in Clinic Assessment of Social Needs Among Caregivers of Pediatric Patients: A Mixed-Methods Study
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 439
Publication Number: 439.489
Publication Number: 439.489

Filoteia Popescu (she/her/hers)
Clinical Research Coordinator III
Vanderbilt University Medical Center
Nashville, Tennessee, United States
Presenting Author(s)
Background: High-quality clinical care alone is insufficient for ensuring optimal patient health outcomes. Recognizing the significant role social determinants of health (SDoH) have in children’s health, the Centers for Medicare & Medicaid Services now requires universal SDoH screening. However, implementation methods vary widely. Although efforts to systemically incorporate SDoH screening are rapidly increasing, little is known about how or if caregivers would like to discuss SDoH during their child’s clinical encounter.
Objective: To conduct a mixed-methods, explanatory sequential approach that evaluates caregivers’ opinions of SDoH screening as part of their child’s pediatric primary care visits.
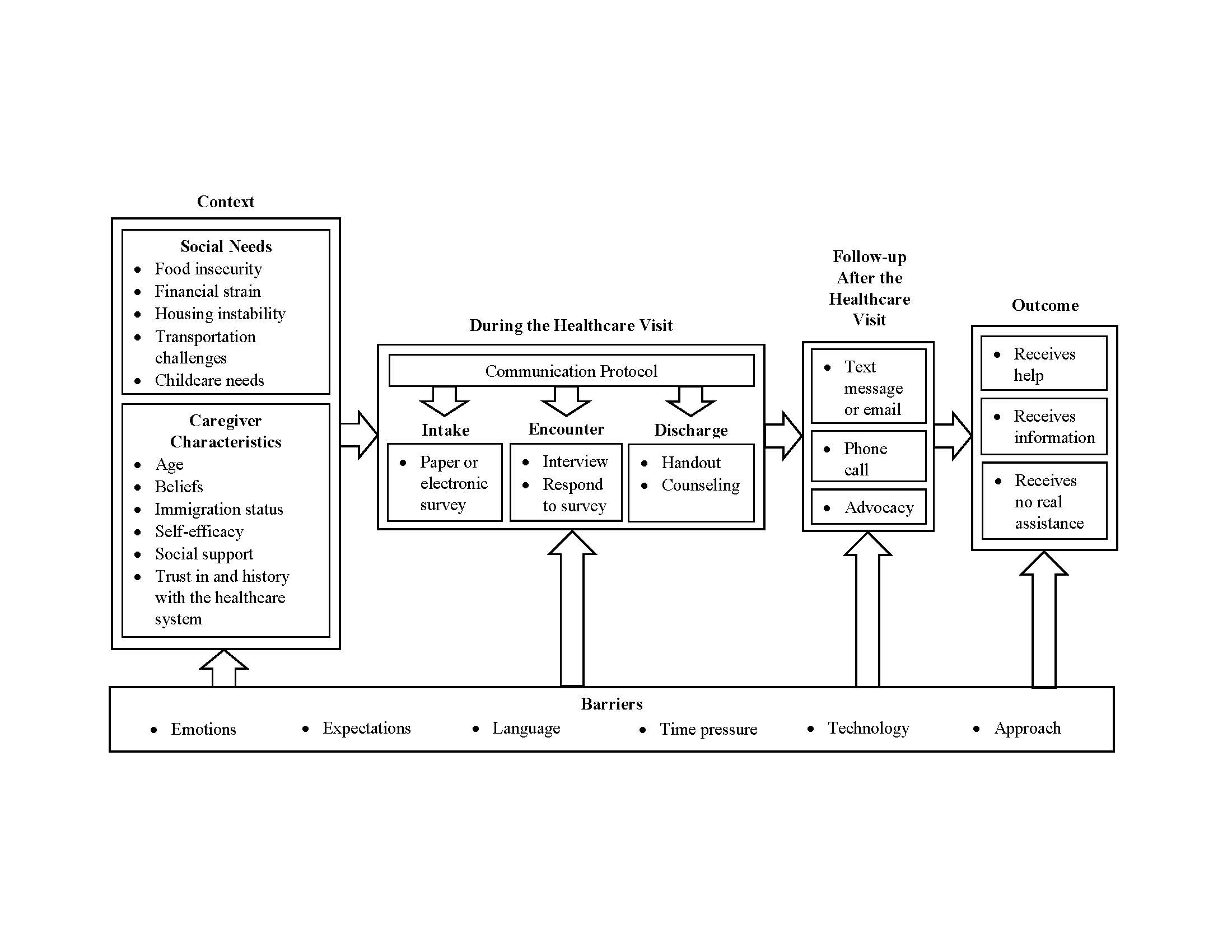
Design/Methods: Quantitative survey data were collected between May 21, 2021, to February 13, 2022, from a convenience sample of 114 caregivers at a primary care clinic that predominantly serves Medicaid-insured patients. Sampled separately, 42 total caregivers participated in six focus groups between February 15, 2022, and March 2, 2022. Eligible caregivers from the Vanderbilt Pediatric Primary Care Clinic were ≥18 years, with a child ≤12 years, and English-, Spanish-, or Arabic-speaking. The primary outcome was caregivers’ interest in SDoH screening, assessed via yes/no response in the quantitative arm and themes coded from transcribed focus groups in the qualitative arm, vetted by multiple coders. A conceptual model emerged illustrating key patient-family barriers and facilitators to their interest in SDoH screening.
Results: Of 114 caregivers surveyed, almost half reported one or more unmet social needs (48%) and most (84%) indicated they did not want to be asked about SDoH in the clinical encounter (Table 1). Qualitative feedback, assessed by grounded theory, revealed domains that affect caregivers’ screening interest. These included the how, who, what, when, and what next of screening (Figure 1). All focus groups identified concerns of being stereotyped, judged, or punished for disclosing unmet needs. Facilitators included utilizing an interpersonal approach, meeting with a clinic staff member the family has a therapeutic relationship with, and setting clear expectations regarding what assistance the clinic can provide for unmet needs.
Conclusion(s): While quantitatively, most participants did not want to be screened for SDoH, qualitative assessment revealed concerns that, if addressed, would improve receptivity. This included asking if they wanted to discuss unmet needs, ensuring a personalized approach with someone they trusted, and clarifying how the health system would address the disclosed unmet needs.
.jpg)
