Neonatology
Session: Neonatal Neurology 7: Neurodevelopment
619 - Perinatal Inflammation Increases Risk of Neurodevelopmental Impairment Among Small for Gestational Age Infants in Bangladesh
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 619
Publication Number: 619.1283
Publication Number: 619.1283

Lian V. Folger, MPH (she/her/hers)
Senior Research Coordinator
Brigham and Women's Hospital
Durham, North Carolina, United States
Presenting Author(s)
Background: 23 million infants are born small for gestational age (SGA) annually, with the majority in low- and middle-income countries. SGA infants carry increased risk for long-term neurodevelopmental impairment. There are limited data on the impact of perinatal inflammation on child neurodevelopment in growth-restricted infants.
Objective: To examine the association between umbilical cord blood inflammatory markers and 24-month neurodevelopmental outcomes among SGA infants.
Design/Methods: Prospective birth cohort study from July 2016–March 2017, following infants until 24 months in Sylhet, Bangladesh. SGA was defined as < 10% birthweight for gestational age and sex based on the Intergrowth-21st standard. Cord blood collected at birth was analyzed for interleukin (IL)-1α, IL-1β, IL-6, IL-8, and C-reactive protein (CRP). Neurodevelopment was assessed at 24 months with Bayley-III Scales of Infant Development. Delay was defined as z-scores < -1. We assessed associations between cord inflammatory marker elevation (>75th%ile vs
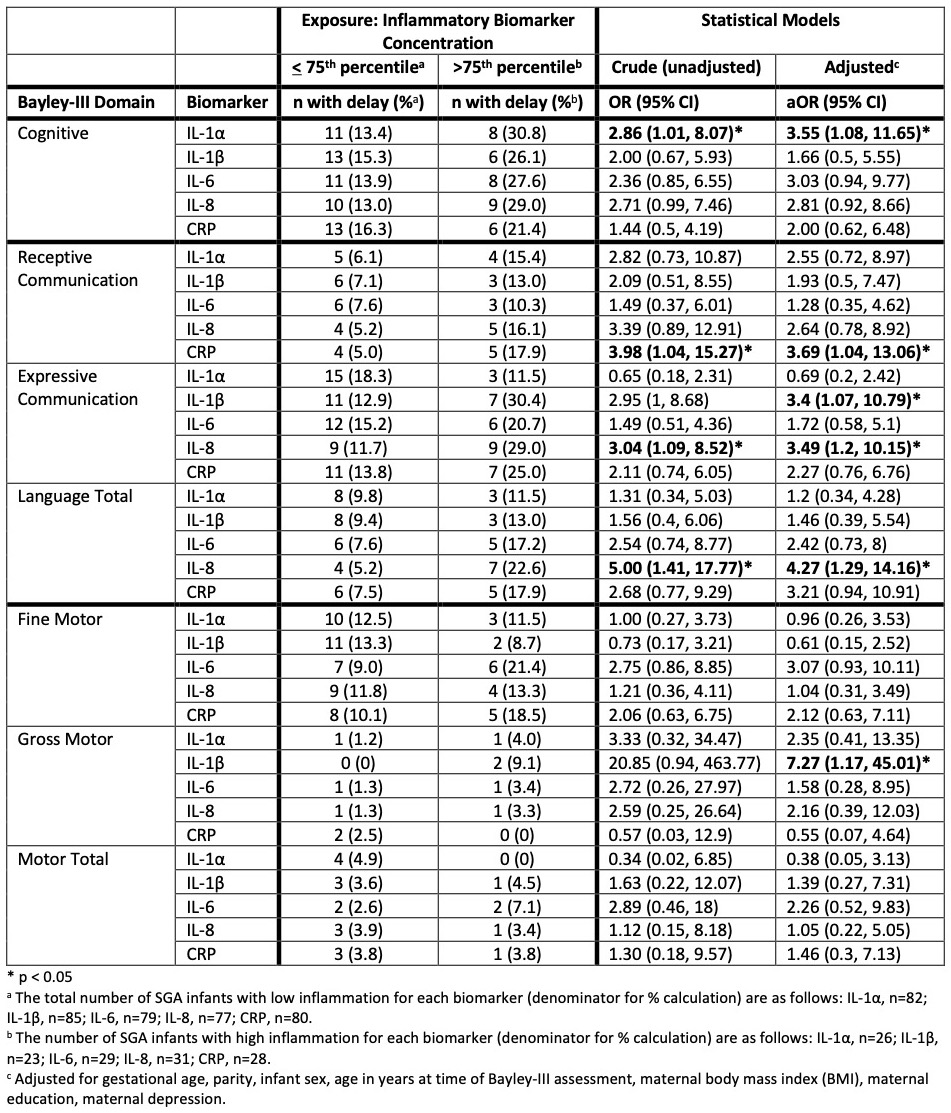
Results: Of 272 infants with birthweight data, 240 (88.2%) were followed until 24 months, among whom 108 (45.0%) were SGA. Among SGA infants, elevated CRP and IL-8 were associated with lower receptive communication z-scores (CRP: -0.48, 95% CI -0.84, -0.13; IL-8: -0.40, 95% CI -0.75 to -0.06) and IL-1β with lower expressive communication (-0.45, 95% CI -0.85, -0.05) and gross motor z-scores (-0.45, 95% CI -0.76, -0.14) (Table 1). IL-1α elevation was associated with higher odds of cognitive delay (adjusted odds ratio [aOR] 3.55, 95% CI 1.08, 11.7), IL-8 elevation with language delay (aOR 4.27, 95% CI 1.29, 14.2), IL-1β elevation with expressive communication delay (aOR 3.40, 95% CI 1.07, 10.8) and gross motor delay (aOR 7.27, 95% CI 1.17, 45.0), and CRP elevation with receptive communication delay (aOR 3.69, 95% CI 1.04, 13.1) (Table 2). Among non-SGA infants (n=132), we observed only one significant association: elevated CRP was associated with higher odds of fine motor delay (aOR 3.7, 95% CI 1.33, 10.3).
Conclusion(s): In rural Bangladesh, perinatal inflammation was associated with developmental delays at 24 months among SGA infants. SGA infants may be more vulnerable to long-term neurodevelopmental impairment due to placental insufficiency, resulting in chronic hypoperfusion, undernutrition, and hypoxia. In this study, we found a consistent pattern demonstrating vulnerability of SGA infants to perinatal inflammation, supporting the neurobiological impact of inflammation in the setting of fetal growth restriction.
.jpg)