Neonatology
Session: Neonatal Neurology 2: Clinical
29 - A prospective study describing splanchnic NIRS values in infants with Neonatal Encephalopathy receiving minimal enteral nutrition during Therapeutic Hypothermia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 29
Publication Number: 29.377
Publication Number: 29.377
.jpg)
Tatiana A. Nuzum, MB BCh BAO (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background: Therapeutic Hypothermia (TH) is the standard of care for moderate-severe neonatal encephalopathy (NE). Historically, minimal enteral nutrition (MEN) has been withheld during TH due to concerns about splanchnic perfusion. Recent observational studies have shown that providing MEN during TH is safe and beneficial. Human milk contains mesenchymal stem cells which are potentially neuroregenerative. Splanchnic regional tissue oxygenation (SrSO2) measured by near-infrared spectroscopy (NIRS) has not been assessed in this population.
Objective: To compare clinical outcomes and SrSO2 levels between infants who received MEN during TH, and those who did not.
Design/Methods: Subjects were prospectively enrolled after informed consent was obtained. Subjects that qualified for TH based on NICHD criteria were eligible. Exclusion criteria included dopamine > 10mcg/kg/min, 2 vasoactive agents simultaneously, and baseline SrSO2 < 45%. Subjects received 10-15 mL/kg/day of expressed or donor human milk for the duration of TH and rewarming. SrSO2 was recorded hourly. Historic controls who were NPO during TH were included after applying the same exclusion criteria. Clinical data for the NICU course was collected.
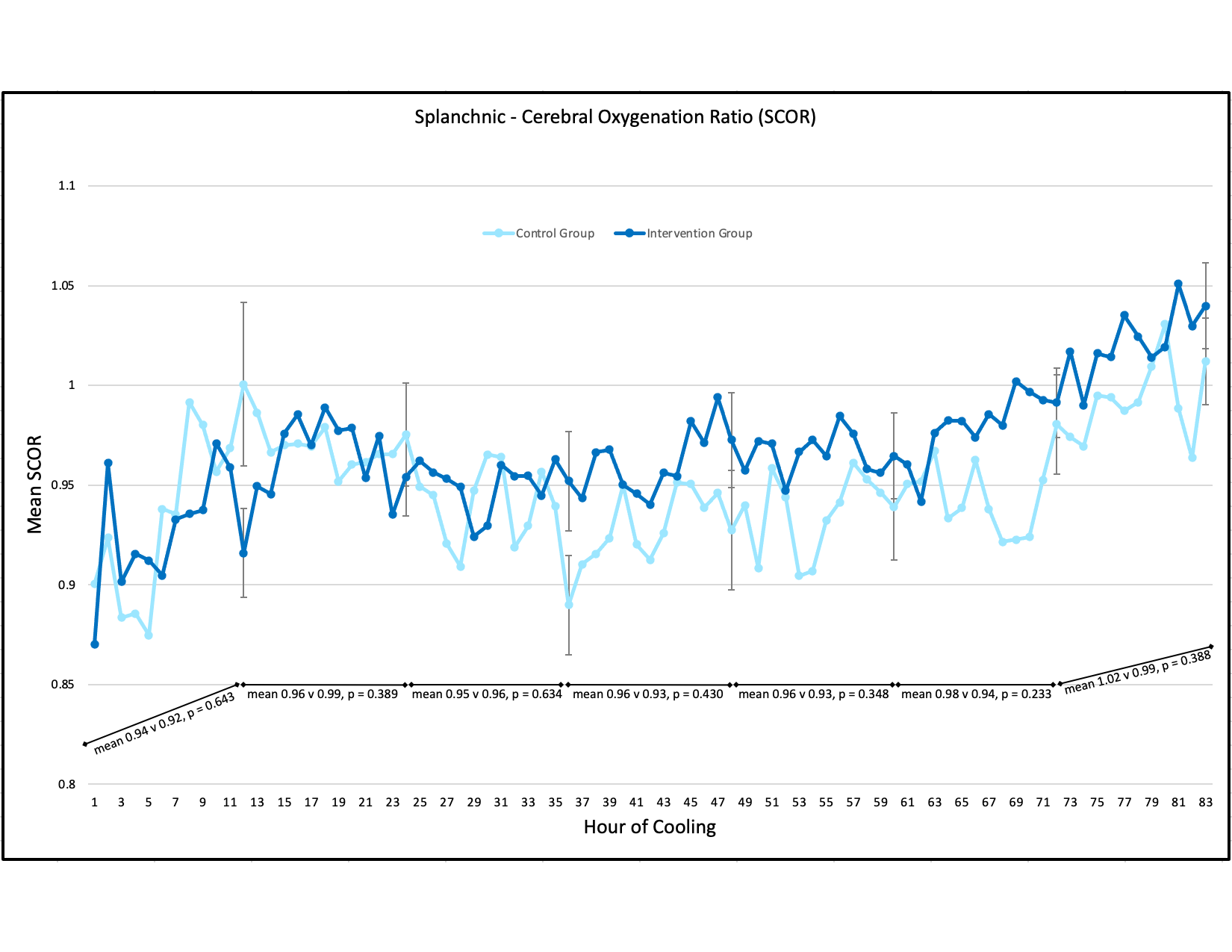
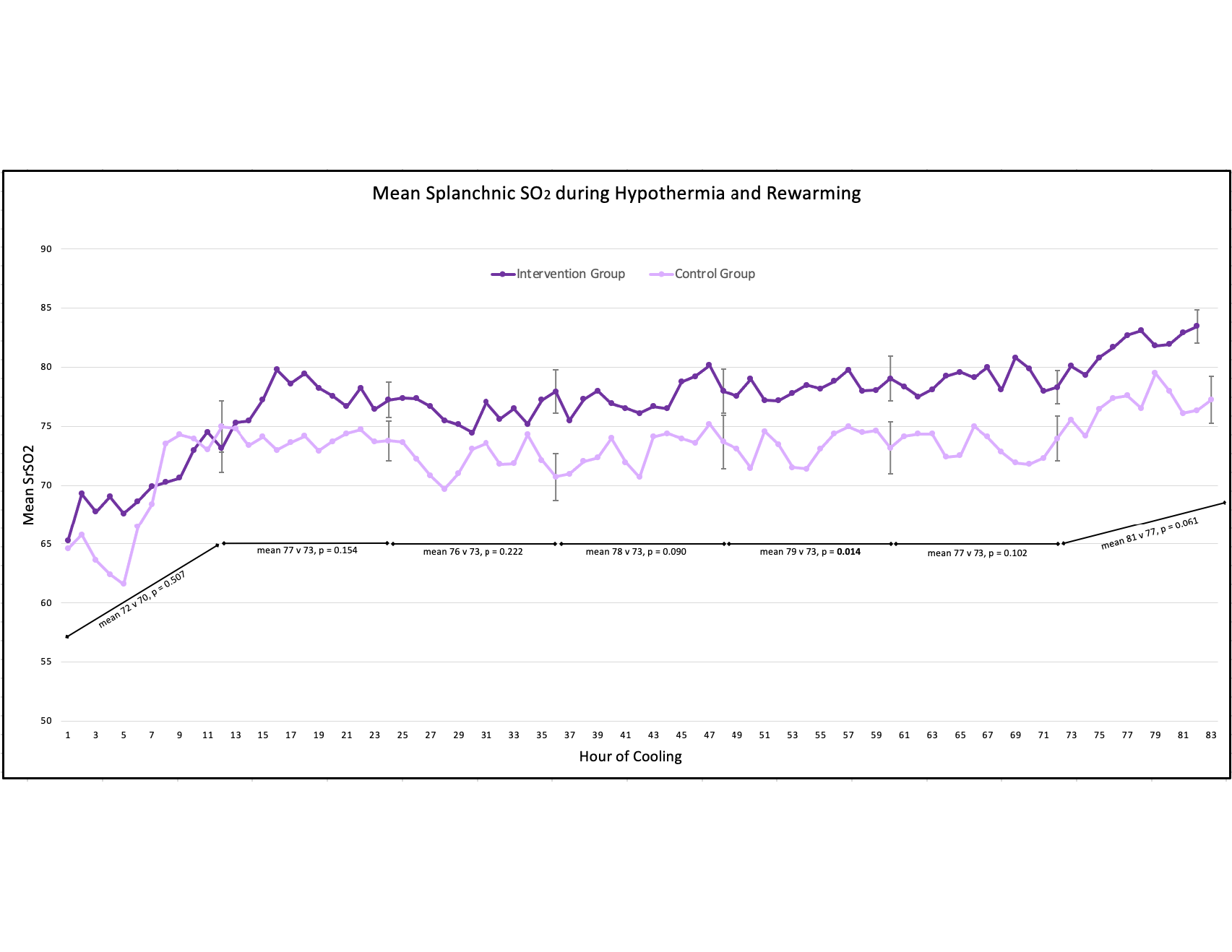
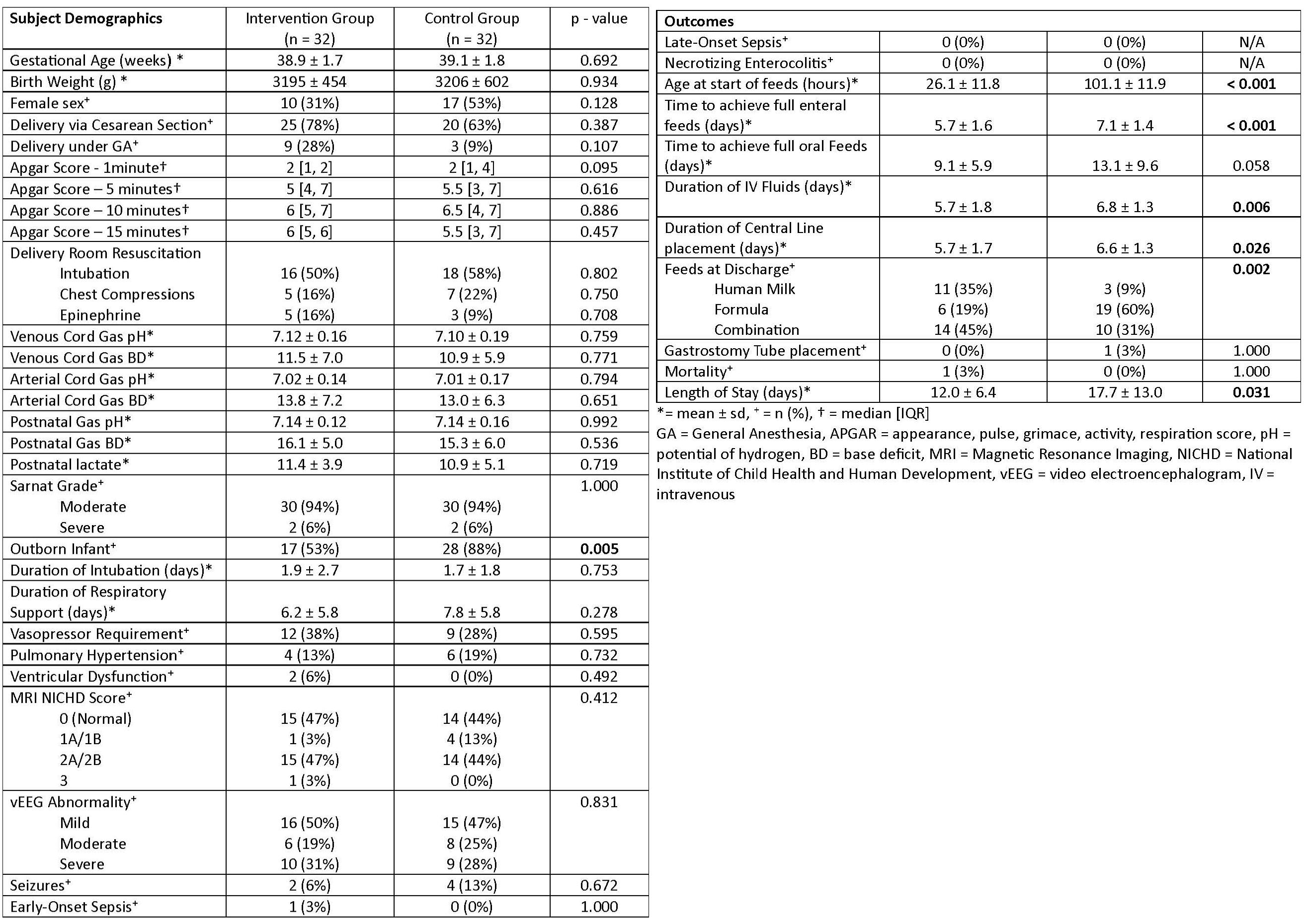
Results: Data was collected for 32 recruits over 1-year and 32 controls. There were no significant differences between the groups at baseline (Table 1). MEN was held in 3 (9%) subjects. One had an upper GI bleed due to stress gastritis from perinatal asphyxia; one had an acute drop in SrSO2 without clinical change, and one had bilious output from gastric tube. MEN was restarted in all three after a period of bowel rest and was well tolerated. Subjects who received MEN experienced fewer central line days (5.7 v 6.6, p = 0.026), shorter hospital stays (12 v 17.7 days, p = 0.031), and a higher proportion of human milk feeding at discharge (80% v 40%, p = 0.002). There was a trend towards subjects who received MEN achieving oral feeds faster (9.1 v 13.1 days, p = 0.058). Mean SrSO2 levels were significantly higher in the intervention group after starting MEN but were within normal ranges in both groups throughout TH and rewarming (Fig. 1). Splanchnic-Cerebral Oxygenation Ratios (SCOR) did not differ between groups (Fig. 2).
Conclusion(s): Splanchnic tissue oxygenation values were within normal ranges throughout hypothermia and rewarming and did not differ between groups. Providing MEN during TH is safe and results in several important benefits including fewer central line days, shorter hospital stays and greater human milk feeding success. Future directions will include assessing long-term neurodevelopmental outcomes.