Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 1
449 - Variability in respiratory support during initial respiratory failure and in-hospital outcomes: Insights from a nationwide US cohort of extremely preterm infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 449
Publication Number: 449.2999
Publication Number: 449.2999

Dominique M. Brandt, MA, MS (she/her/hers)
Health Economics Policy and Reimbursement Analyst
Medtronic
Cincinnati, Ohio, United States
Presenting Author(s)
Background: The initial respiratory support strategies for extremely low gestational age neonates (ELGANs) has been gradually evolving from invasive mechanical ventilation (IV) to non-invasive ventilation (NIV) resulting in variability in the practice. The impact of different respiratory supports on long term outcomes is not clear, more so in lower gestational age infants.
Objective: To investigate the prevalence of different respiratory support strategies used during the first 14d of life and their association with in-hospital outcomes in ELGANs.
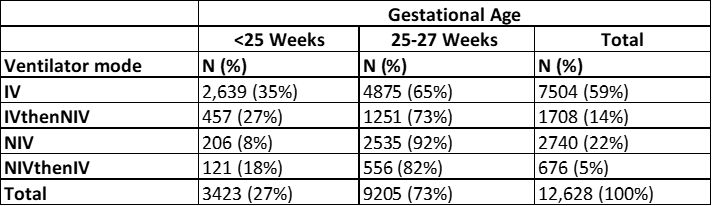
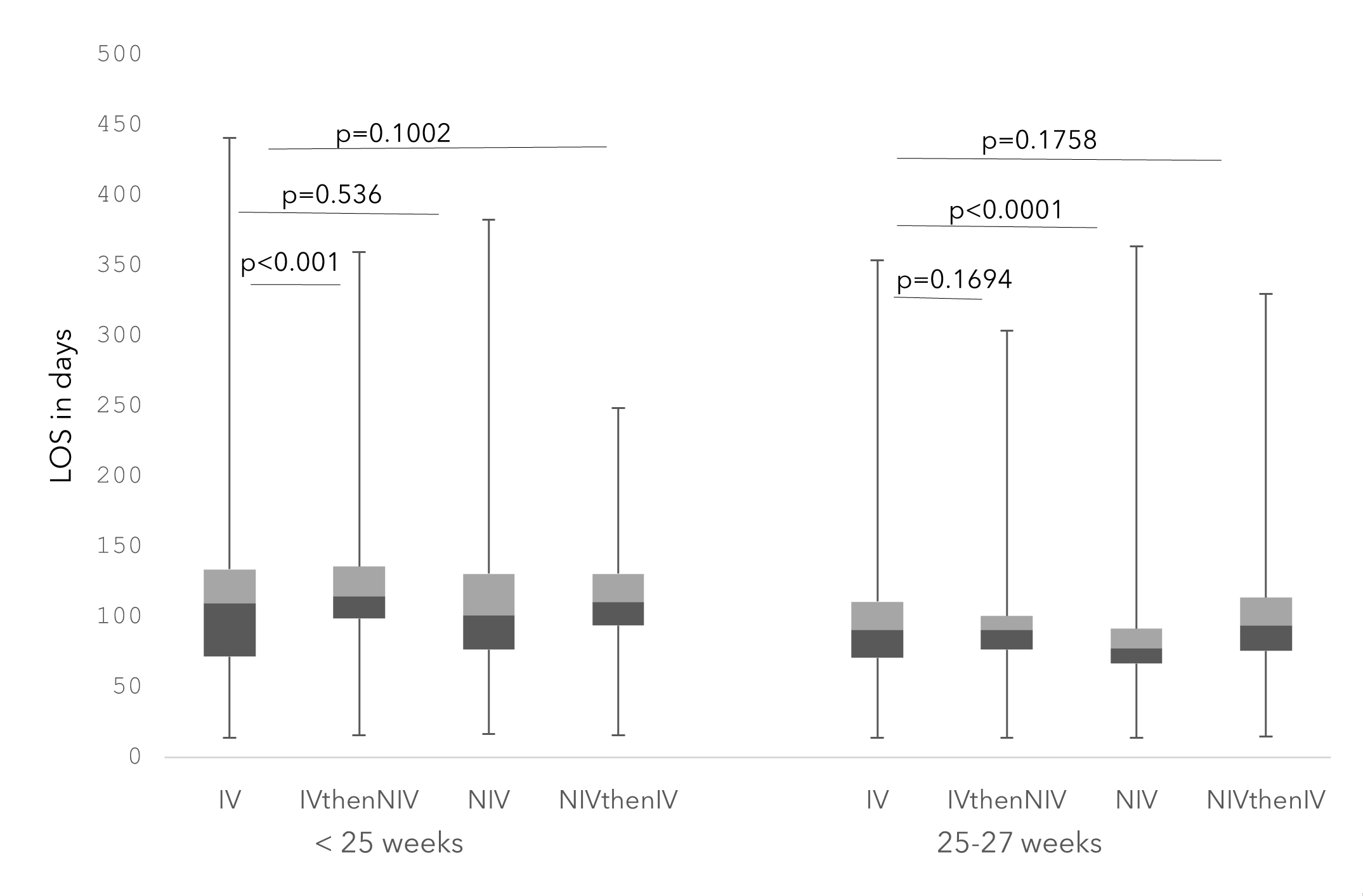
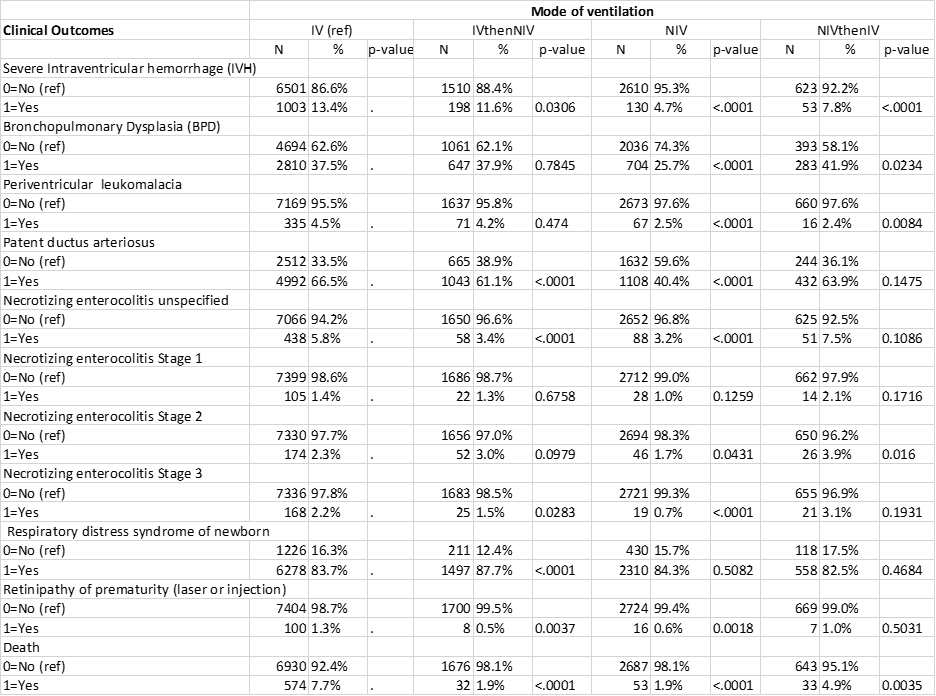
Design/Methods: This is a retrospective cohort study of the Premier Healthcare Database, which is a large all-payer service-level US-hospitals database. All Infants born between 2017-21 at < 28w GA who survived beyond 14d and received respiratory support identified by ICD-10 PCS codes were included in the analysis. Infants were divided into four groups according to the sequence of respiratory support received during the first 14d: IV, NIV, IV then NIV, or NIV then IV. In-hospital outcomes were compared between the four groups with further stratification in two groups according to GA. Outcomes of interest were length of hospital stay (LOS), diagnoses at discharge and survival. LOS among GA groups and modes of ventilation and outcomes at discharge were compared using generalized linear model (GLM) method.
Results: Out of 12,628 infants meeting the study criteria, 3423 (27%) were born at < 25w. Overall, 7504 (59%) received IV and 22% received only NIV for first 14d. Only 6% of infants at < 25w GA received NIV for 14d, as compared to 28% in 25-27w group. Infants on IV only had a higher LOS than NIV if born 25-27 weeks GA (Tbl2). Overall, outcomes at discharge were worse in IV infants with a mortality of 7.7% vs. 1.9% in IV then NIV P< 0.0001, 1.9% NIV p< 0.0001 and 4.9% NIV then IV, p=0.0035. Worse outcomes in IV vs NIV infants were found for IVH, BDP, PVL PDA, p < 0.0001. The incidence of ROP was significantly lower in NIV then IV 0.6% vs. 1.3%, p=0.0018, and vs. IV then NIV 0.5% p=0.0035 but not for NIV then IV 1%, p=0.5031 (tbl3).
Conclusion(s): Despite concerted efforts by the clinicians, majority of ELGANs receive IV during first 2 weeks with only 6% of those born < 25w receiving exclusive NIV. Since NIV is associated with improved clinical outcomes, there is an urgent need to devise newer innovative strategies to avoid IV in ELGANs.