Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 2
464 - Survey of Late Preterm Care Practices within a Large Neonatal Network
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 464
Publication Number: 464.3014
Publication Number: 464.3014

Elizabeth Salazar, MD (she/her/hers)
Instructor
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Late preterm infants (34 0/7 to 36 6/7 weeks GA [gestational age]) represent over 70% of preterm births in the United States; yet, the variability surrounding their optimal care practices remains unknown.
Objective: To describe the provider-level variation in late preterm care practices within greater Philadelphia neonatal intensive care units (NICUs) including hospitals in Philadelphia, South Jersey, and Delaware.
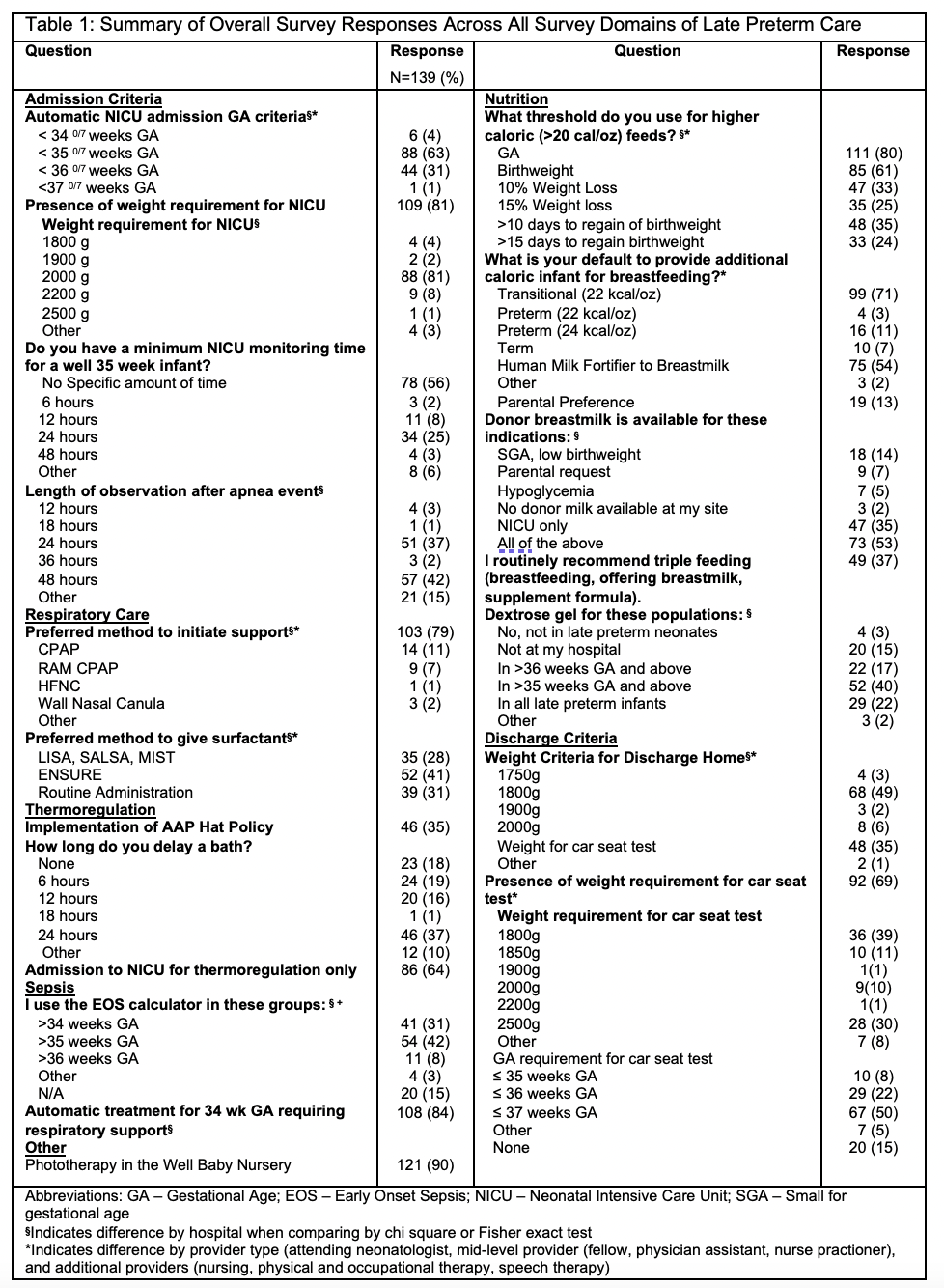
Design/Methods: In October 2023, we administered a 31-item online survey of late preterm care practices to NICU providers among 18 NICUs. Providers practiced at level II, III, and IV units. We obtained data from the following domains: admission criteria, discharge criteria, respiratory management, nutrition, infectious management, and thermoregulation. We used chi square and fisher exact tests with a threshold of p < 0.05 to identify differences in responses between hospitals and provider types.
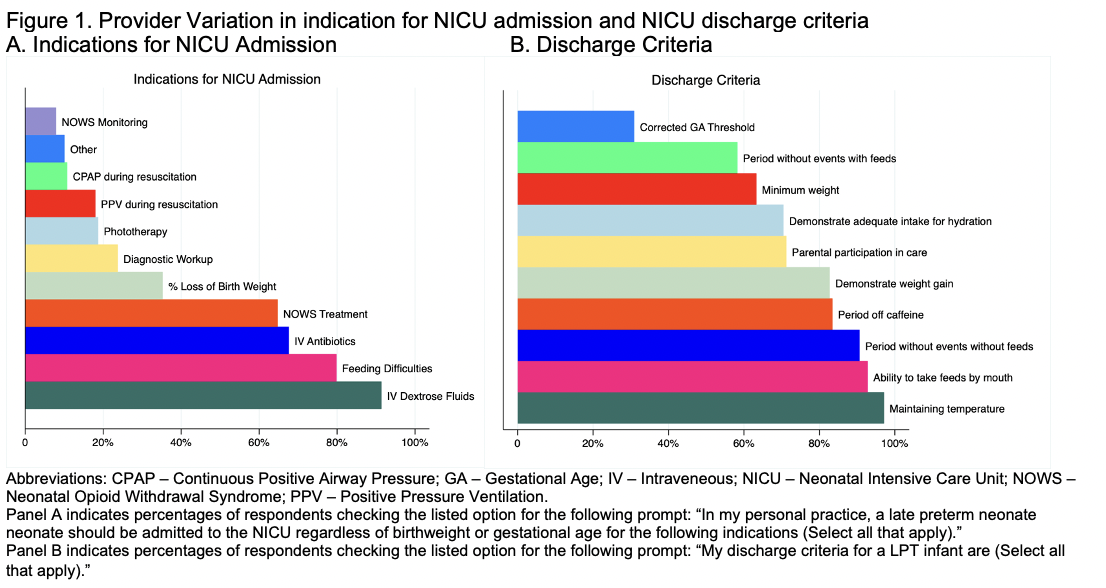
Results: We received 139 responses from 17 NICUs (estimated response rate 55%), including 70 attending neonatologists (50%), 24 fellows, nurse practioners, physician assistants, or hospitalists (17%), and 34 additional providers (24%). There was substantial provider-level variability in across all survey domains (Table 1), including in indications for admission and discharge criteria (Figure 1). There were significant differences between hospitals among the following variables: admission gestational age and birthweight, need for NICU admission for IV antibiotics and monitoring for neonatal opioid withdrawal syndrome, the observation period for apnea, preferred respiratory support, preferred surfactant administration method, indication for surfactant and supplementation, use of donor milk and dextrose gel, discharge criteria and weight, and use of the early onset sepsis calculator and sepsis management (Table 1, Figure 2 A-C). Between provider types, there were significant differences in automatic GA for admission, preferred form of respiratory support, preferred surfactant administration method, and discharge weight criteria (Table 1, Figure 2 D-E).
Conclusion(s): In this preliminary, single region survey of late preterm care practices, wide variation existed in management of multiple aspects of care, including admission and discharge criteria, respiratory management, and nutrition. Further national data are needed to both understand patterns of national variation in late preterm care as well as drivers of unnecessary and harmful variation in care.
.png)
