Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
43 - A Multidisciplinary Quality Improvement Initiative to Improve the Komansky Children's Hospital's Emergency Escalation System
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 43
Publication Number: 43.2719
Publication Number: 43.2719
- MT
Megan Toal, MD (she/her/hers)
PCCM Attending
Weill Cornell Medicine
Brooklyn, New York, United States
Presenting Author(s)
Background: Rapid Response Team (RRT) activation occurs when a patient demonstrates early signs of deterioration. RRT is composed of a team of responders capable of supplying critical resources and performing interventions at a moment’s notice at the patients’ current location. Recently, in our medical surgical units we have experienced an increase in the number of hospitalizations of medically complex patients, including those who are technology supported (e.g. tracheostomy, feeding tubes). These patients are at risk of rapid deterioration requiring provider prompt activation of RRT. Our baseline Adverse Event data have shown a significant delay in RRT activation leading to an increased number of Preventable Adverse Events (PAE).
Objective: On medical surgical units we aimed to 1) reduce the number of PAEs to zero and 2) improve healthcare providers’ comfort with escalating care by 20% by June 2023.
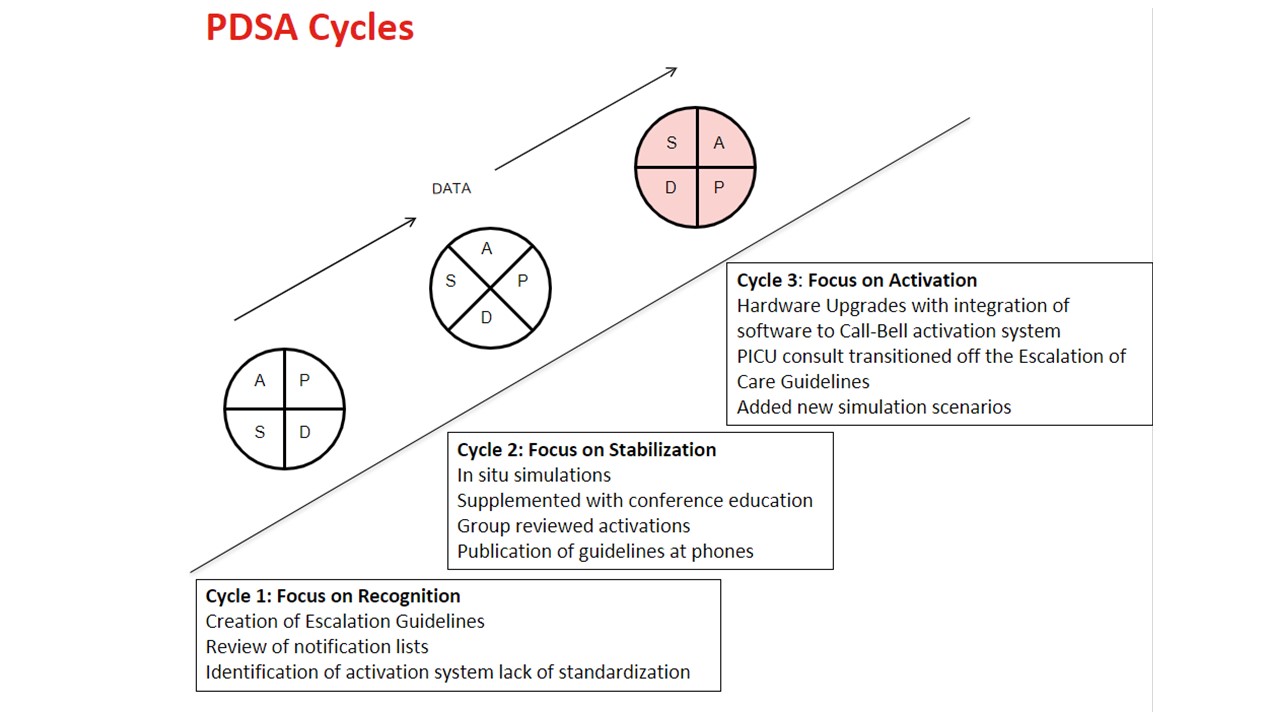
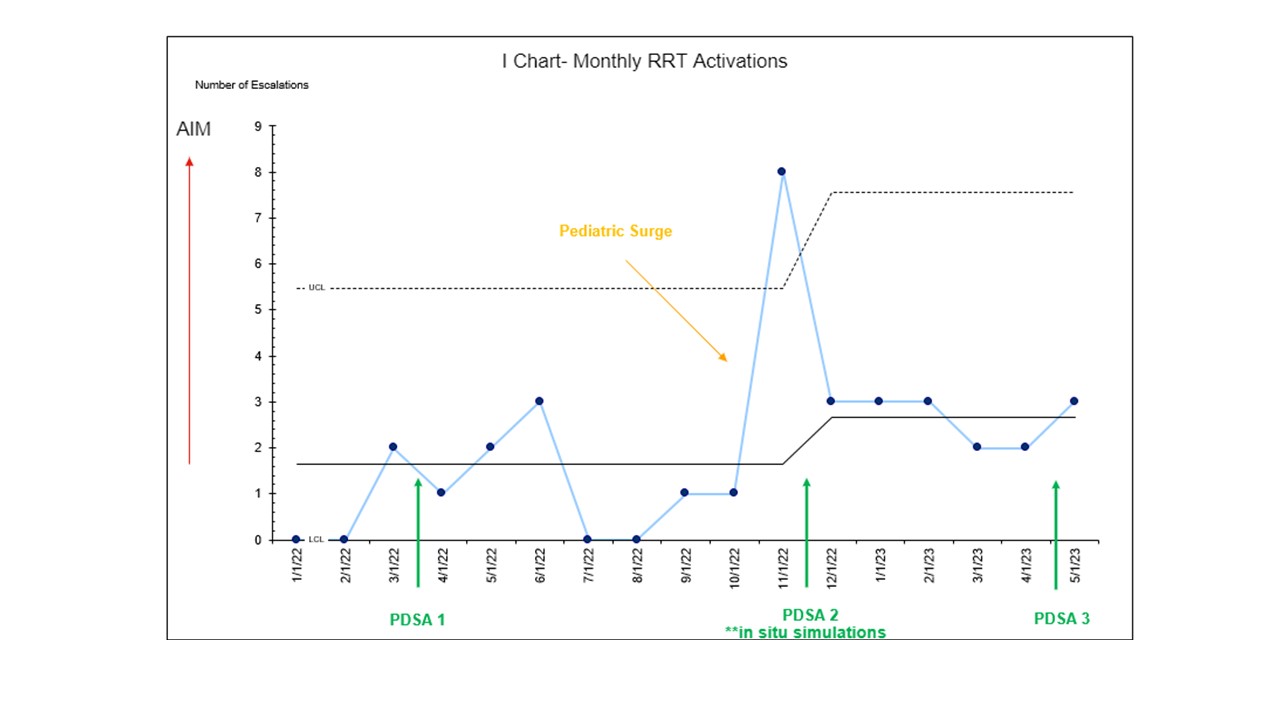
Design/Methods: Using the Model for Improvement, a series of sequential interventions were implemented as listed in Figure 1. Our outcome measures included the number of PAEs on the medical surgical units related to escalation of care and to follow self-reported comfort level with RRT activation. We utilized the following process measures including the number of providers who participated in interdisciplinary in-situ simulations of RRT activation and the number of monthly RRT activations. The number of activations that do not lead to pediatric intensive care unit (PICU) transfer were collected as a balancing measure. Data were collected via electronic medical record (EMR) review and analyzed using statistical process control charts. We applied API rules to detect special cause variation.
Results: We improved the monthly RRT activation rate from 1.5 to 3.5 (Figure 2). In addition, provider’s self-reported comfort in RRT activation improved from 63% to 93%, an increase of 30%. To date we experienced 1 PAE. We completed a total of five in-situ simulations in which there was 50% resident (n = 60) , 30% nursing (n = 100), 50% respiratory therapy (n = 4), and 100% of pharmacy staff participation (n = 2). There was no increase in activations that did not lead to PICU transfer.
Conclusion(s): We demonstrated a successful multifaceted approach to increasing provider’s comfort level to activate RRT for medically complex patients who are showing early signs of deterioration. In situ simulation using clinical scenarios was the most impactful intervention.