Emergency Medicine
Session: Emergency Medicine 3: Serious Bacterial Infections
99 - Prevalence of positive urine culture with negative urinalysis in well-appearing febrile infants 22-90 days old regarding biomarkers
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 99
Publication Number: 99.1311
Publication Number: 99.1311
.jpg)
José Antonio Alonso Cadenas (he/him/his)
Pediatric Emergency Physician
Pediatric Emergency Department. Niño Jesús University Hospital
Madrid, Madrid, Spain
Presenting Author(s)
Background: The 2021 Clinical Practice Guideline of the American Academy of Pediatrics for the management of febrile infants aged 8 to 60 days old recommends not collecting a urine culture (UC) when urinalysis is negative. In these cases, positive UC results are likely to represent asymptomatic bacteriuria or contamination. Blood tests [procalcitonin (PCT), C-reactive protein (CRP), and absolute neutrophil count (ANC)] identify infants at higher risk for bacterial infection, so we hypothesized that their values could be considered to decide the need of obtaining a UC in these patients.
Objective: To compare the rate of positive UC in well-appearing febrile infants 22-90 days old with a normal urinalysis in patients with normal and altered blood tests (PCT, CRP and ANC).
Design/Methods: Sub-study of a multicentre retrospective study including infants 0-90 days old with fever without a source attended at two Spanish pediatric emergency departments (ED) between 2011 and 2021. For the purpose of this subanalysis, we included all well-appearing infants 22-90 days old with normal urinalysis, and PCT, CRP, ANC, blood culture (BC) and a UC obtained by a sterile technique. We compared the rate of positive UC (≥10 000 cfu/mL by urethral catheterization; ≥100 000 cfu/mL by clean-catch technique) in patients with normal (PCT < 0.5 ng/mL, CRP ≤20 mg/L and ANC ≤10 000/mcL) or altered biomarkers. Invasive bacterial infection (IBI) was defined as the isolation of a bacterial pathogen in blood or cerebrospinal fluid.
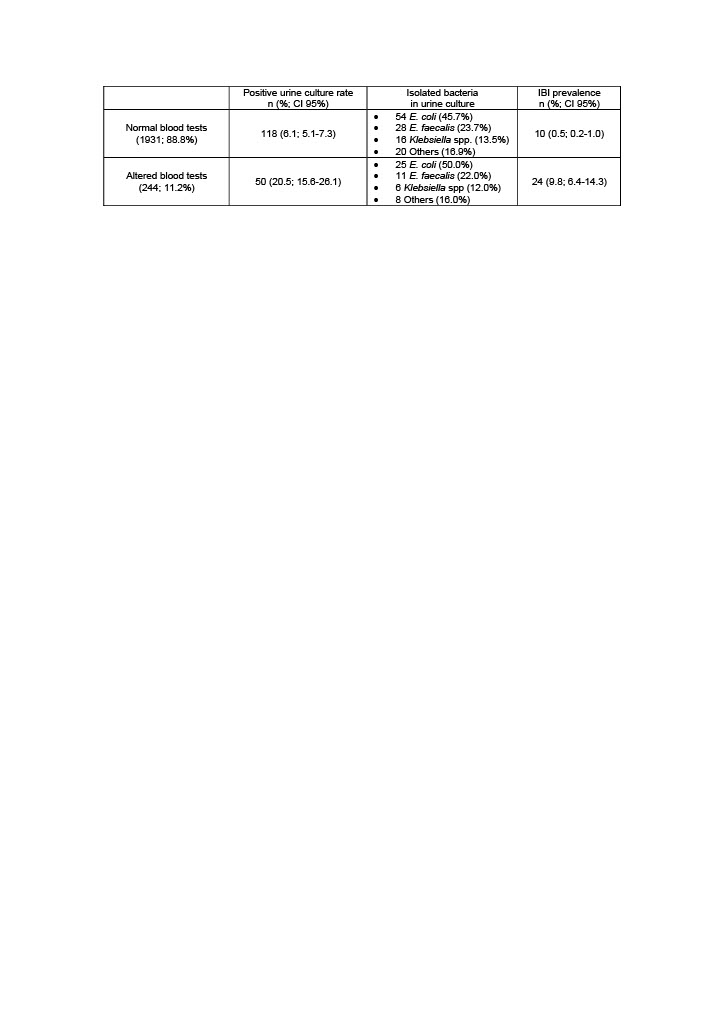
Results: Among 3415 well-appearing infants 22-90 days old, 2677 (78.4%) had a normal urinalysis. Of them, 2175 infants (81.2%) met the inclusion criteria and were included in this subanalysis. The UC was positive in 168 (7.7%). Overall, main isolated microorganisms in UC were E. coli (79, 47.0%), E. faecalis (39, 23.2%), and Klebsiella spp (22, 13.1%). The rate of positive UC was significantly higher in those patients with altered biomarkers, without differences in the distribution of isolated bacteria (Table 1). Only one patient diagnosed with an IBI had a positive UC for the same bacteria (S. agalactiae; normal blood tests).
Conclusion(s): Among well-appearing febrile infants 22-90 days old and normal urinalysis, those presenting elevated blood tests values have a significantly higher rate of positive UC. This finding suggests that a proportion of them could have a true UTI instead of an asymptomatic bacteriuria. UC may be considered to be collected in these infants and mid-term management should be individualized.