Neonatology
Session: Neonatal/Infant Resuscitation 3
299 - Statewide Neonatal Readiness Assessment at Delivery Hospitals in Maine
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 299
Publication Number: 299.2912
Publication Number: 299.2912

Misty Melendi, MD (she/her/hers)
Division Chief, Neonatology
The Barbara Bush Children's Hospital at Maine Medical Center
Portland, Maine, United States
Presenting Author(s)
Background: In Maine, the most rural state in the United States, more than two-thirds of hospitals deliver less than one neonate per day. Neonatal mortality has been shown to be higher in hospitals with low birth rates. Therefore, understanding neonatal readiness is vital when developing initiatives to address this outcome disparity.
Objective: We aimed to understand neonatal readiness at delivery hospitals statewide to identify where neonatal preparedness is lacking to assist in prioritization of statewide educational and outreach initiatives to delivery hospitals.
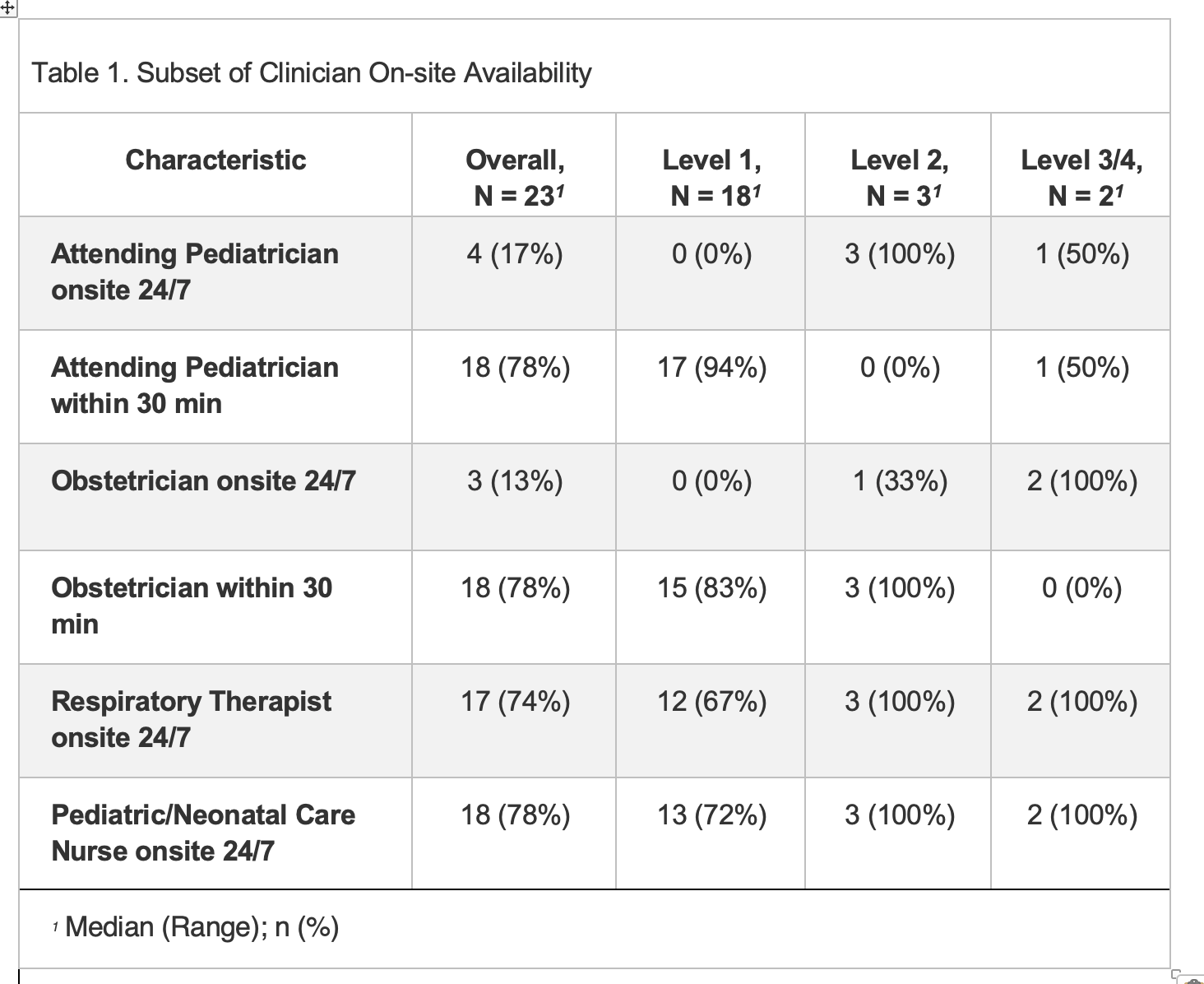
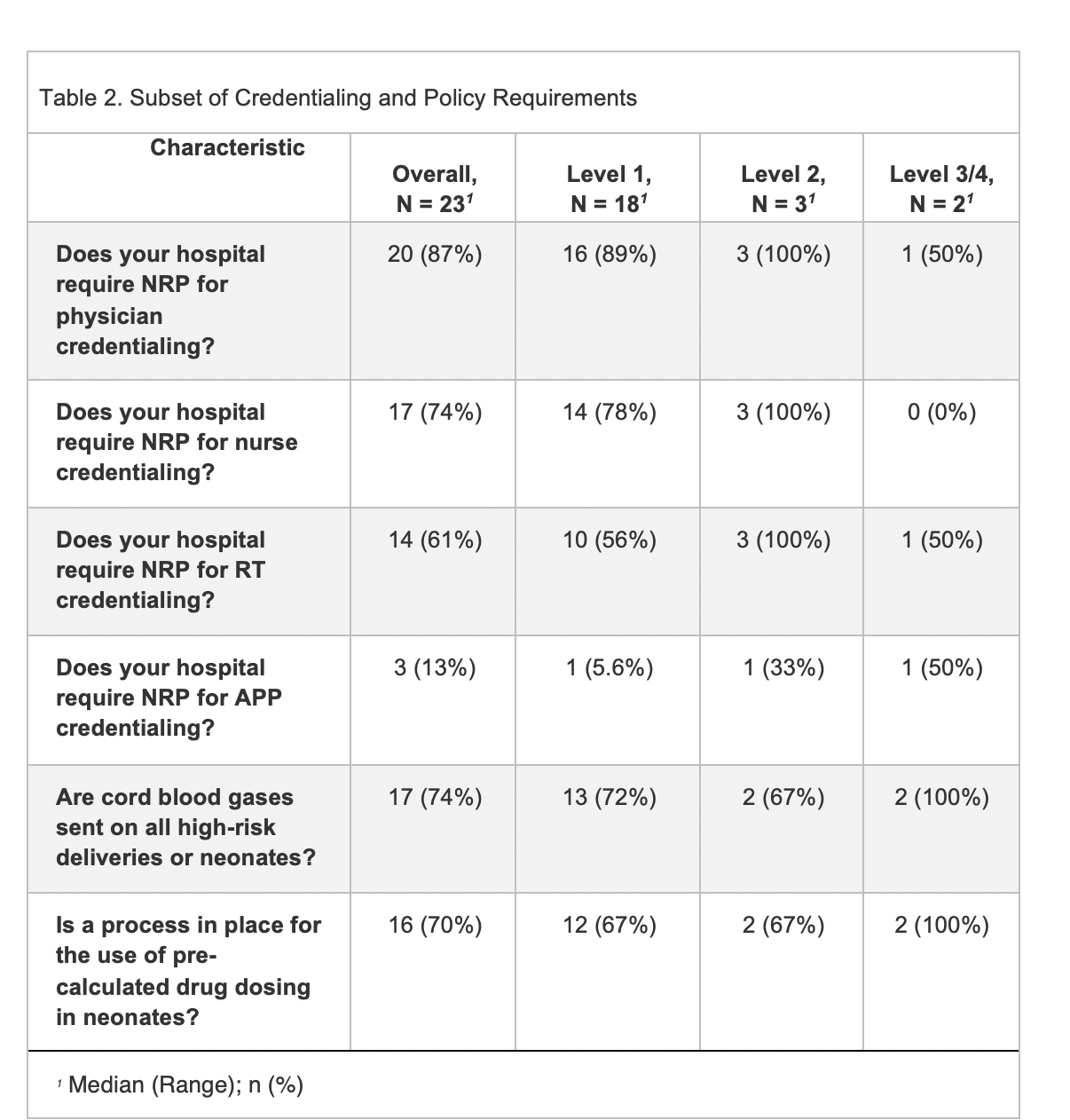
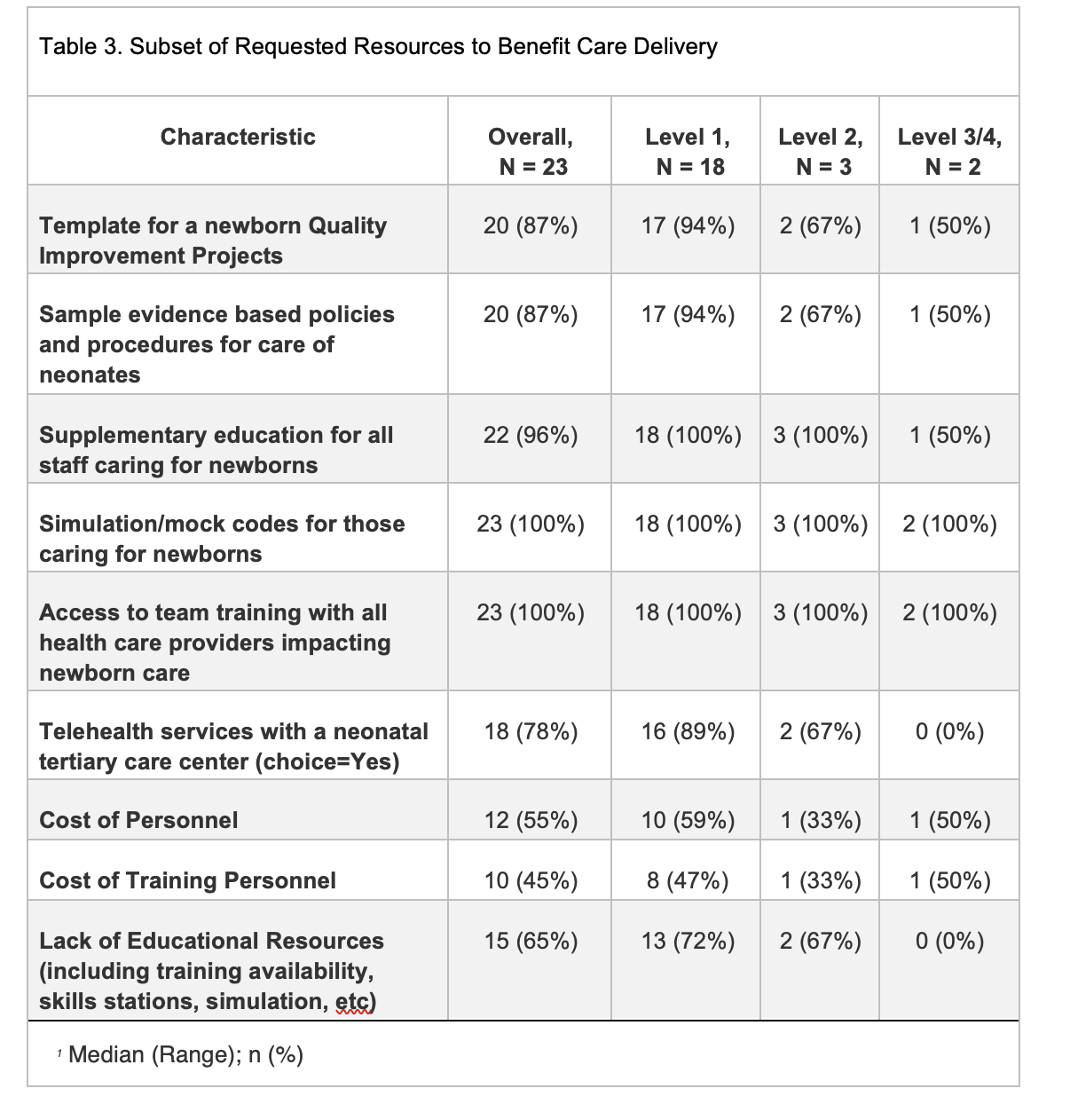
Design/Methods: A mixed methods design was utilized including a comprehensive survey and interviews completed with clinical leads at each delivery hospital in Maine. A subset of survey sections included hospital infrastructure, services, personnel, training, leadership, policies, transport preparedness, and equipment. The survey also asked about barriers to and resources for improving neonatal care delivery. Data was stratified by state-designated level of care into three groups: Level I, Level II, and Levels III/IV to represent tertiary hospitals.
Results: All birthing hospitals open as of May 2022 participated in the study, including 18 Level I, 3 Level II, 1 Level III, and 1 Level IV hospitals. Sites were enrolled from May 2022-September 2023. Few sites report having an on-site Pediatrician (17%) and Obstetrician (13%). Most Level I/II hospitals do not have access to on-site pediatric specialists but report having access to specialists via phone. Overall, 87% of hospitals require NRP training for neonatal physicians, 74% for nurses, 61% for respiratory therapists, and 22% for APPs. A total of 17 hospitals report requiring cord blood gases to be sent on high risk deliveries and 16 have a process for pre-calculated drug dosing. Site-level qualitative data was collected from clinical leads, with a recurring theme of a need for additional training opportunities.
Conclusion(s): Additional support from tertiary hospitals to Level I/II hospitals is urgently needed, including obtaining appropriate equipment, availability of telephone consults/telemedicine with specialists, and medical director oversight. Four participating delivery hospitals have since closed to deliveries, emphasizing the crisis facing rural hospitals in newborn preparedness. This trend is worrisome due to the creation of maternity deserts and immediate educational and clinical support is needed to keep delivery hospitals open and improve preparedness for neonatal resuscitation.