Neonatology
Session: Neonatal Pulmonology - Clinical Science 4: Clinical Practice Questions, Going Home
570 - Use of long-term home ventilation for preterm infants with bronchopulmonary dysplasia in British Columbia: a retrospective cohort study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 570
Publication Number: 570.2854
Publication Number: 570.2854

Kudrat Mundi, BSN (she/her/hers)
Medical Student
UBC Faculty of Medicine
Cawston, British Columbia, Canada
Presenting Author(s)
Background: Improved survival at increasingly low gestational ages (GA) has resulted in a growing population of infants with bronchopulmonary dysplasia (BPD). In cases of severe BPD, ongoing respiratory support may be needed after neonatal unit (NICU) discharge. Treatment options include low-flow oxygen (LFO2), non-invasive ventilation (NIV), and ventilation via tracheostomy (trach/vent).
Objective: To characterize the population of infants with BPD who require respiratory support after NICU discharge, and describe trajectory including long-term clinical outcomes and differences in outcomes according to type of home respiratory support.
Design/Methods: Retrospective study of infants ≤32 weeks GA with BPD and use of respiratory support at NICU discharge in British Columbia, 2013-2022. Cases were identified from hospital coding and provincial NICU follow-up and home ventilation patient databases. Serial growth and neurodevelopmental measures were collected at 4, 8, and 18 months corrected age, 3 and 4.5 years.
Results: 102 infants with BPD (66% male, 22% multiple birth) were discharged on home respiratory support. Median GA was 25 weeks and birthweight 727g. Home support was with trach/vent in 9% (n=9), NIV in 39% (n=40), and LFO2 in 52% (n=53). Median corrected age at tracheostomy insertion was 3.8 months.
Characteristics of children in NIV and trach/vent groups were similar, apart from a higher prevalence of medically managed pulmonary hypertension and older age at successful extubation in the trach/vent group (Table 1).
Infants with trach/vent were older at NICU discharge (median 391 vs 210 days, p< 0.001) and stopping ventilation (median 4.6 vs 1.7 years, p< 0.001) than those discharged on NIV. In LFO2 treated children, median age at stopping O2 was 9 months.
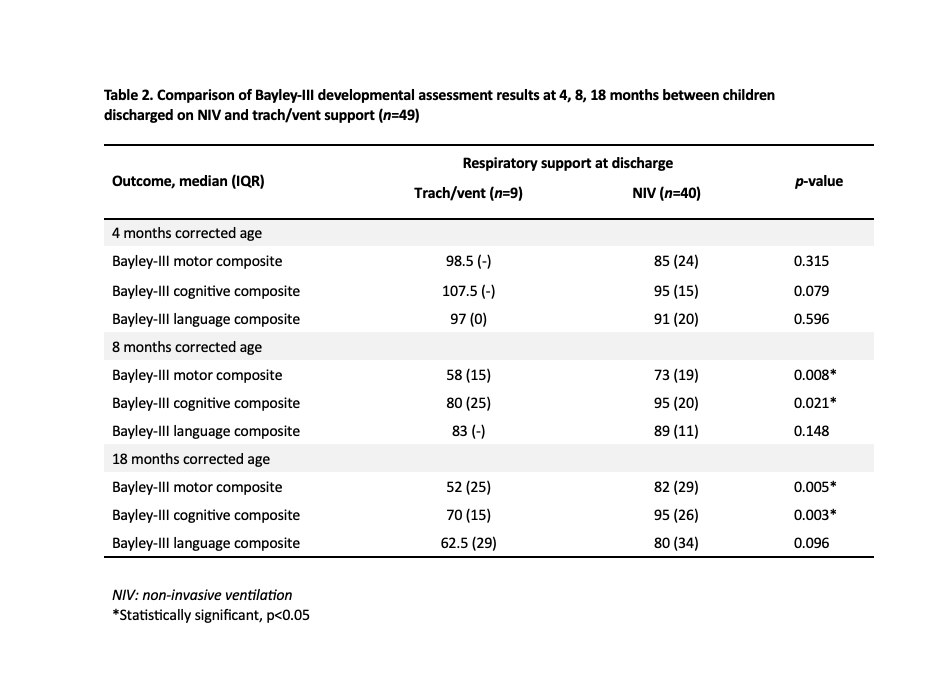
Bayley-III scale cognitive and motor composite scores were similar in infants supported with NIV and trach/vent at 4 months, but significantly lower in the trach/vent group at 8 and 18 months (Table 2). There was no difference in median weight-for-age z-scores between the two groups at any time point.
Hospital readmission within 2 years of NICU discharge was more common in infants with trach/vent than NIV (89% vs 62%). All children were alive at median 4.5 years follow-up.
Conclusion(s): Use of home NIV to support infants with BPD is associated with shorter NICU admission and ventilation duration than trach/vent. No advantages of trach/vent over NIV were identified in terms of neurodevelopment or growth. These findings endorse use of home NIV in infants with BPD assuming they are not fully ventilator dependent.
.jpg)