Neonatology
Session: Neonatal Pulmonology - Clinical Science 6: Respiratory/Neuro Outcomes, Steroids
593 - Early Extubation in Extremely Preterm Infants: Impact on Neonatal Outcomes
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 593
Publication Number: 593.2831
Publication Number: 593.2831
- KB
Kari G. Bruce, MD (she/her/hers)
Neonatologist
UC Irvine/CHOC Children’s
Ladera Ranch, California, United States
Presenting Author(s)
Background: Invasive ventilation (via endotracheal tube) is a major risk factor for the development of bronchopulmonary dysplasia (BPD) in preterm infants. Early extubation in extremely preterm (EPT; < 27 weeks’ gestation) infants is perceived as risky due to concern for morbidities associated with extubation failure.
Objective: To examine if early extubation (within the first 3 days of life) in EPT infants increases the risk of mortality and morbidities, particularly severe intraventricular hemorrhage (IVH).
Design/Methods: This is a retrospective chart review of EPT infants born between 22 – 26 weeks’ gestation from 1/1/2013 to 12/31/2018 at the University of California Irvine Medical Center. Patient demographics including gestational age (GA) and birthweight (BW), respiratory characteristics, and short-term outcomes were evaluated. Extubation was deemed successful if an infant remained extubated for >72 hours.
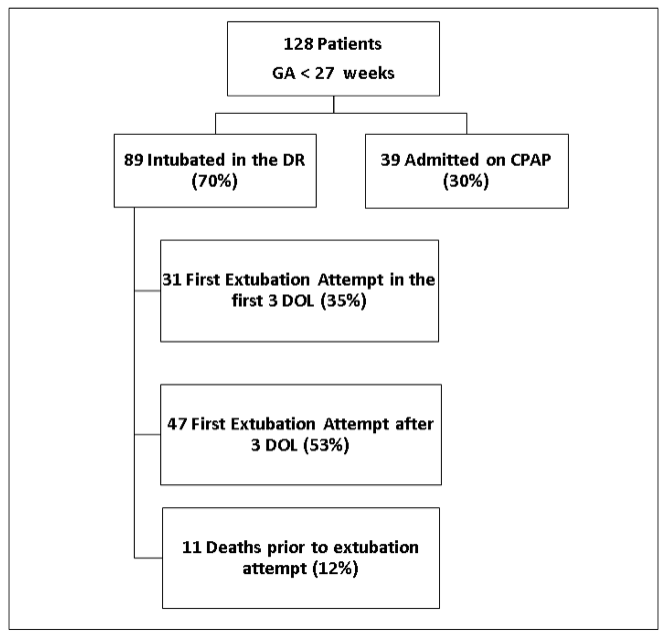
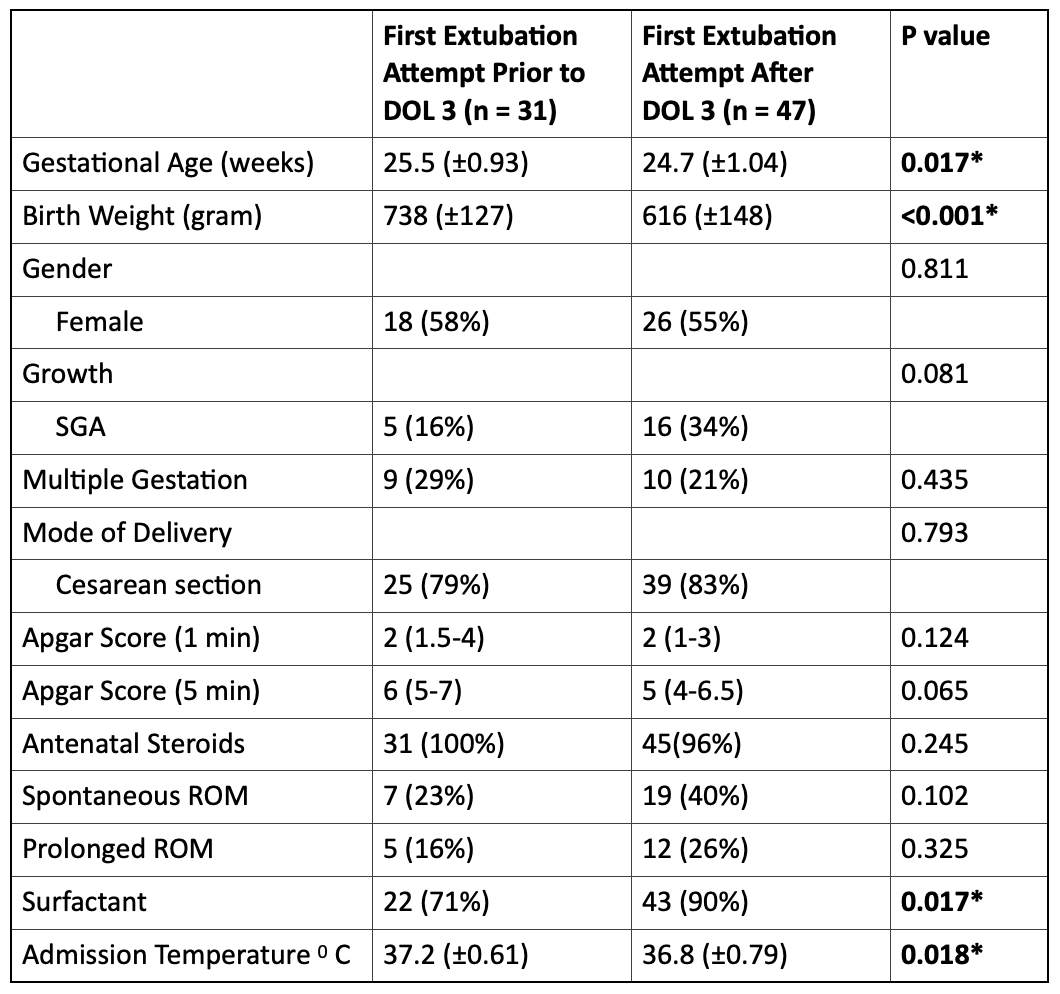
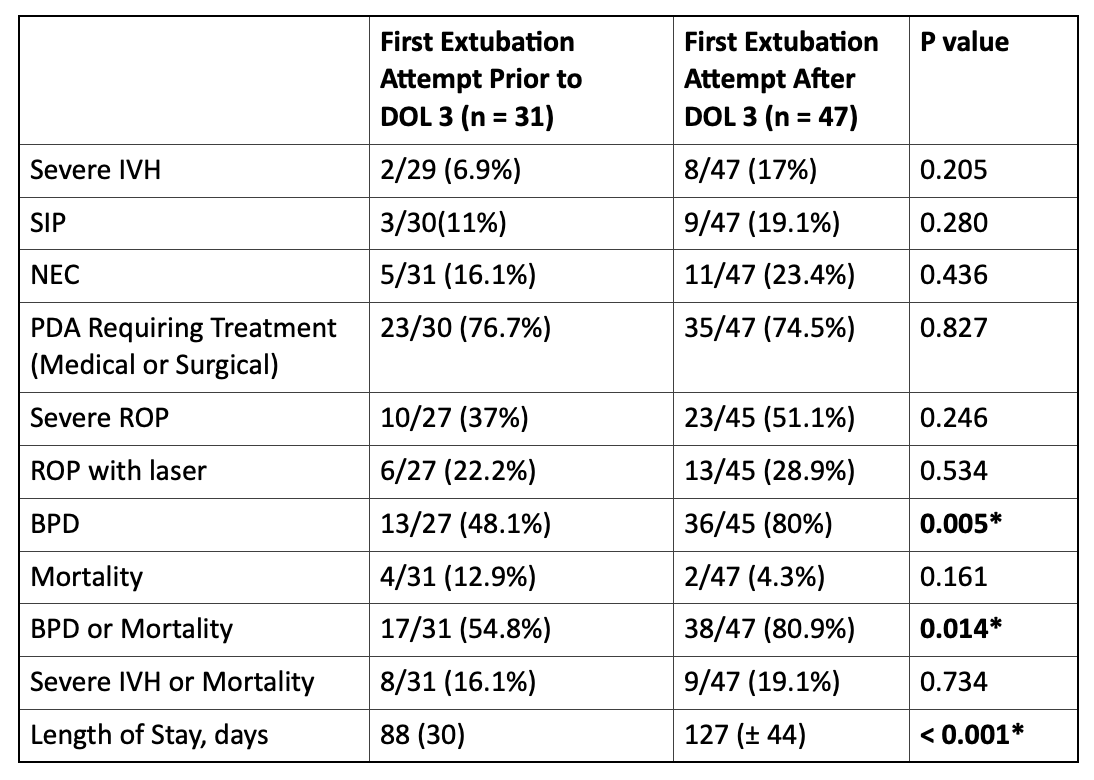
Results: A total of 128 inborn were evaluated for the study. Eighty-nine were intubated in the delivery room, of which 11 infants died without the opportunity for a trial of extubation. Among the remaining 78 patients; 31 had first extubation attempt in the first 3 days of life (group 1) and 47 after the first 3 days of life (group 2). Group 1 patients had a higher GA (25.5 ± 0.93 vs 24.7 ± 1.04, p=0.017) and a higher BW (738 ±127 vs 616 ±148 g, p=0.0002). Infants in group 2 were more likely to be on high frequency oscillatory ventilation, to have a higher mean airway pressure/PEEP and were more likely to have a higher PaCO prior to extubation. The rate of successful extubation was similar between the two groups (61% for group 1 vs 68% for group 2, p=0.537). There was no difference in severe IVH, patent ductus arteriosus requiring therapy, necrotizing enterocolitis, spontaneous intestinal perforation, retinopathy of prematurity or mortality between the two groups. Group 2 patients were more likely to have a longer length of stay, and more likely to have a higher incidence of BPD and BPD/death. Logistic regression analysis continued to show significantly longer length of hospital stay in group 2 patients after adjusting for BW, GA, and other variables.
Conclusion(s): Early extubation in EPT infants appears to be safe and not associated with increased morbidities or mortality. Extubation after day of life 3 in this population may increase the risk of BPD, BPD/death and is associated with a longer length of hospital stay.