Neonatology
Session: Neonatal/Infant Resuscitation 1
269 - Title: Evaluation of a respiratory care protocol including less invasive surfactant administration in 30-34 weeks’ GA infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 269
Publication Number: 269.2791
Publication Number: 269.2791
- SA
Swathi Ariyapadi, MD (she/her/hers)
Pediatric Resident
UC irvine
Irvine, California, United States
Presenting Author(s)
Background: Less Invasive Surfactant Administration (LISA) decreases the need for mechanical ventilation (MV) and improves outcomes in preterm infants. Large randomized controlled trials evaluating LISA included infants born ≤28 weeks gestational age (GA). The benefits of LISA over endotracheal surfactant administration in moderate to late preterm infants is not well established. Starting Oct 2018, Parkland Health & Hospital System (PHHS) implemented the OPTISURF bundle consisting of stepwise escalation of CPAP from 5 to 7 cm H2O followed by LISA guided by fractional inspired oxygen (FiO2) ≥0.3. Compared to a historical cohort, PHHS reported decreased need for MV within 72 hours of life (HOL) and pneumothorax after implementing the bundle in infants ≤ 29 weeks GA.
Objective: To evaluate the effects of the OPTISURF bundle in 30-34 week GA infants. The primary outcome of interest is the need for MV within 72 HOL
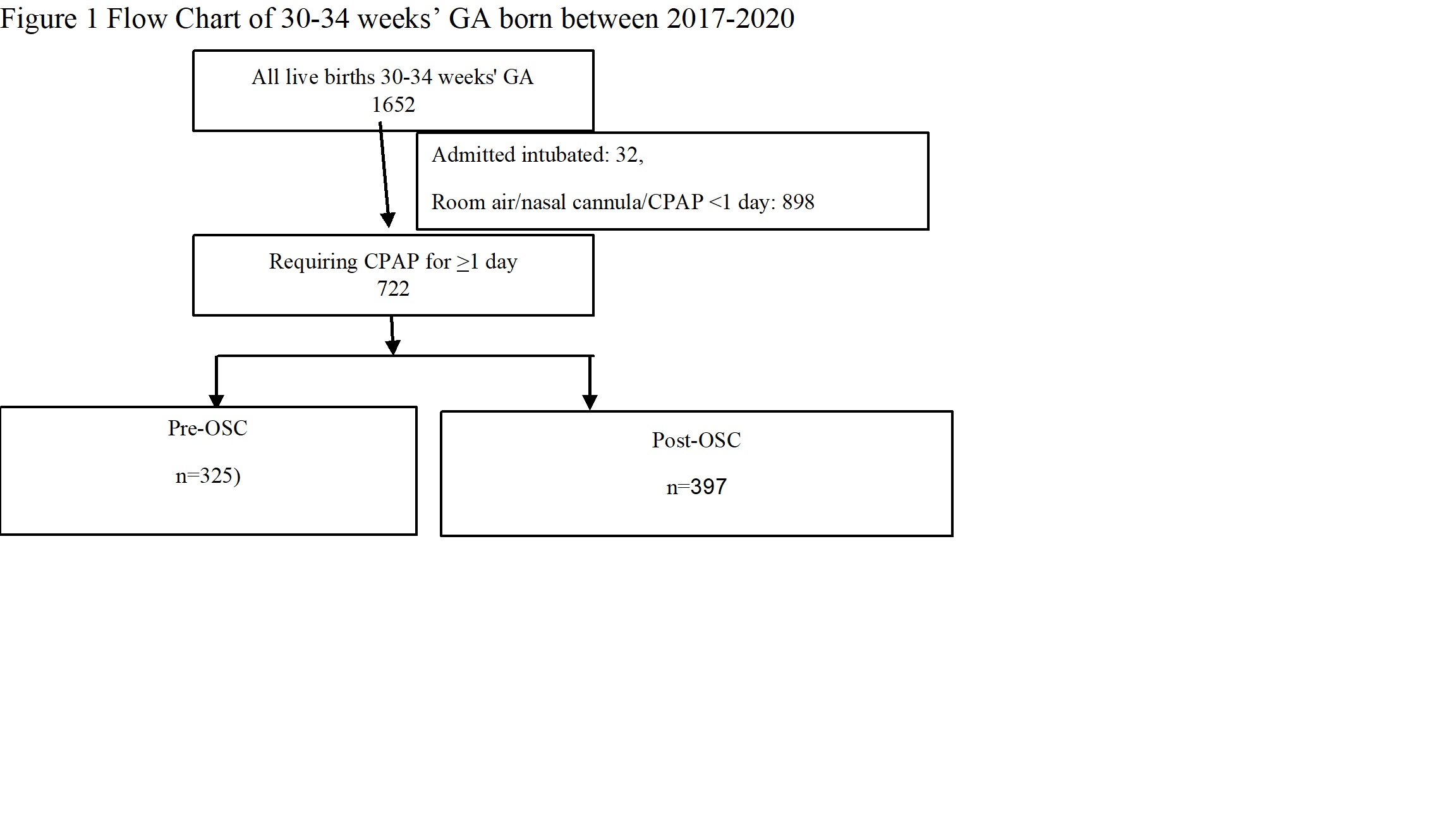
Design/Methods: This is a single center retrospective study of 30-34 week GA infants born between Jan 2017 and Dec 2020 requiring CPAP for ≥ 1 day during hospital stay. Maternal and neonatal variables were compared between the group of infants born prior to implementation of OPTISURF [Jan 2017-Sept 2018, pre-OPTISURF cohort (OSC)] and after implementation (Oct 2018-Dec 2020, post-OSC)
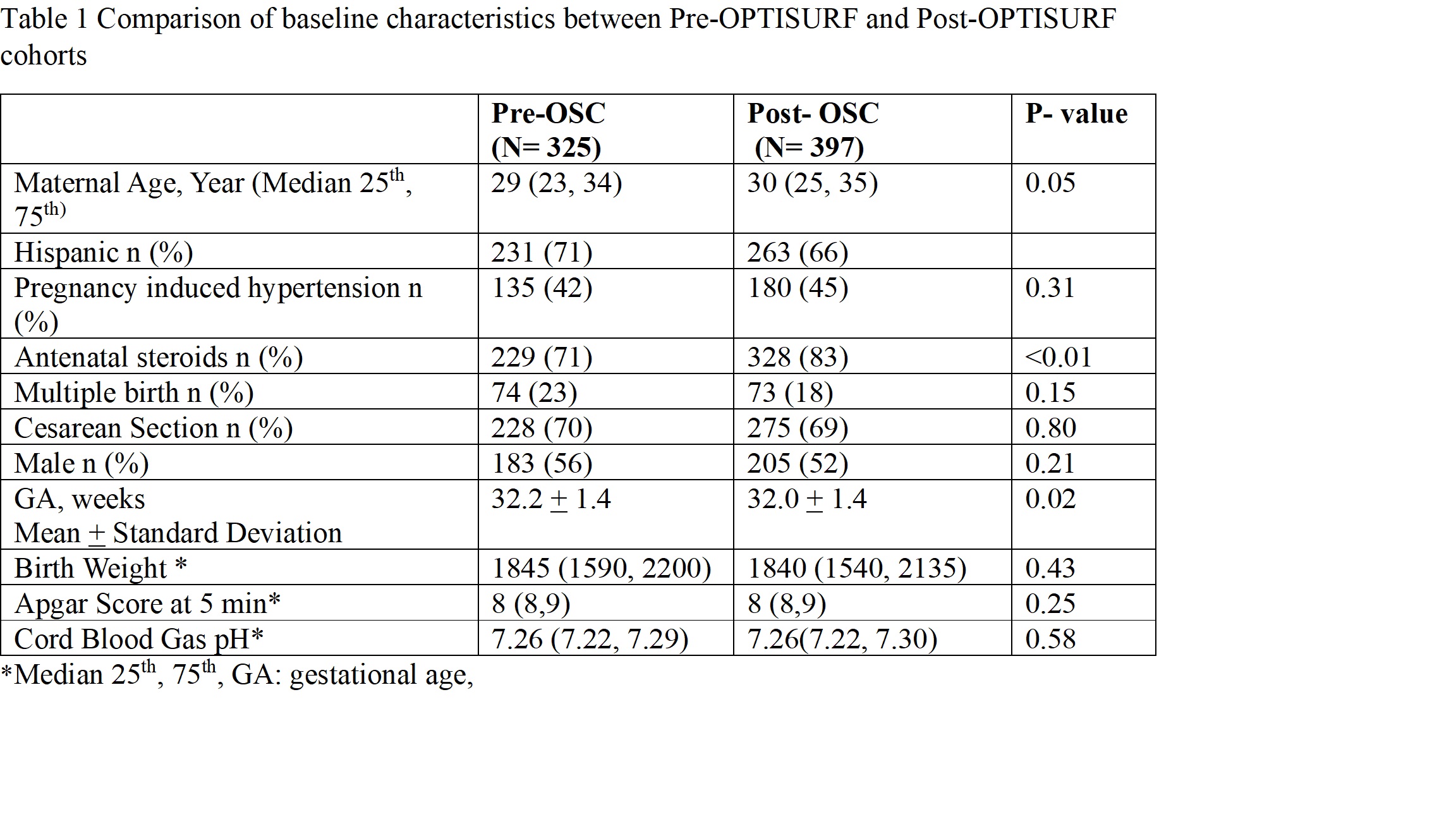
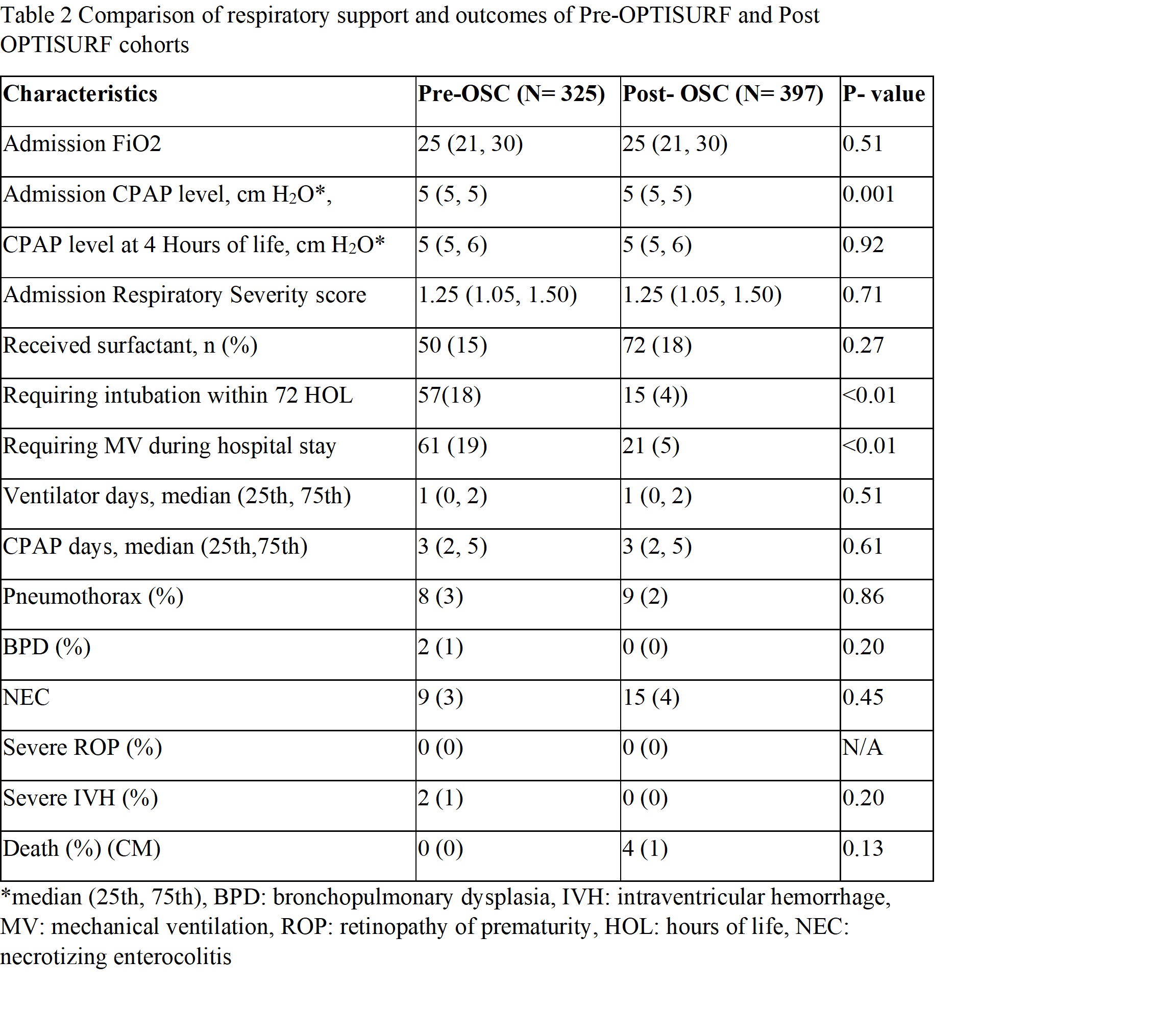
Results: Of the 722 infants requiring CPAP ≥ 1 day, 325 infants belonged to pre-OSC and 397 to post-OSC (Fig 1). There was no difference in the baseline maternal and neonatal characteristics except for higher exposure to antenatal steroid and lower average GA among post-OSC infants (Table 1). There was no difference in admission FiO2 between groups. Although CPAP level on admission was higher in the post-OSC, FiO2 and respiratory severity score was not different between the two cohorts. The need for MV within 72 HOL and during the hospital stay were lower in the post-OSC compared to pre-OSC. However, the length of hospital stay was longer in the post-OSC compared to pre-OSC. There were no differences in any other outcomes between two cohorts (Table 2).
Conclusion(s): A respiratory care protocol consisting of stepwise escalation of CPAP guided by FiO2 ≥0.3 and LISA decreased the need for MV within 72 HOL and during the hospital stay but did not improve any other outcomes.