Neonatology
Session: Neonatal GI Physiology & NEC 1: Necrotizing Enterocolitis
519 - Standardizing Adjunct Abdominal Ultrasound for the Diagnosis of Necrotizing Enterocolitis May Mitigate NEC Severity
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 519
Publication Number: 519.2188
Publication Number: 519.2188

Clifford Hegedus, MD
Fellow
Medical University of South Carolina
Charleston, South Carolina, United States
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) remains a highly morbid disease for preterm infants. Clinicians predominantly rely on abdominal radiography to diagnose NEC. The use of abdominal ultrasonography (AUS) improves the evaluation of early or uncertain cases of NEC.
Objective: To determine if universal implementation of AUS utilized as an adjunct tool for the diagnosis of NEC improves the frequency of detecting abdominal findings consistent with NEC as compared to a 10-year cohort (2010-2020). We also assessed the severity of NEC before and after the implementation of this protocol using a current 2-year baseline.
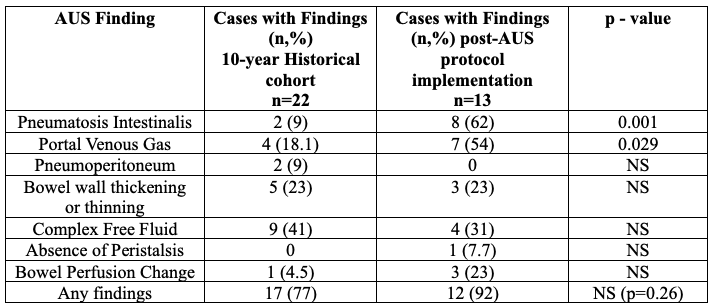
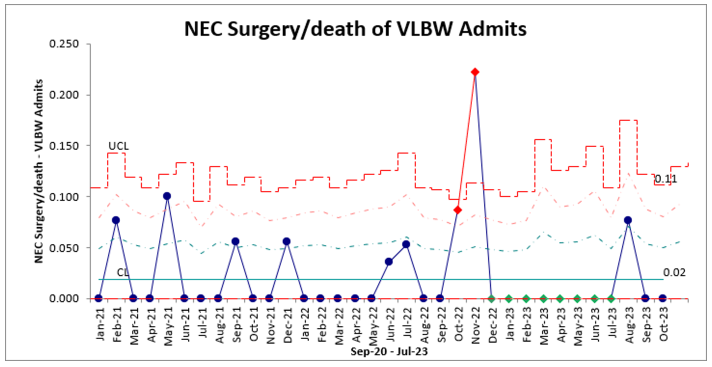
Design/Methods: Data was collected from our Level IV, 82-bed neonatal intensive care unit (NICU) from January 2021-October 2023. Confirmed NEC was defined as Modified Bell Stage 2A or greater. A standardized AUS report template was designed to report on seven specific findings suggestive of NEC (Table 1). Unit guidelines for the management of NEC were updated in February 2023 to recommend clinicians universally obtain an AUS during every initial workup of NEC as an adjunct to abdominal radiography. AUS findings were examined post-implementation and compared to the historical cohort. A comparison of the rates of surgical NEC before (January 2021-January 2023) and after (February 2023-October 2023) was performed using a Chi-squared test. Significance was p < 0.05.
Results: In the two years prior to AUS protocol implementation, there were 11 surgical NEC/deaths of 27 total cases (38%). Post-implementation, there have been 13 cases of NEC. All of these cases received AUS during the initial workup. The overall NEC rate (medical or surgical) was unchanged (7.5%). Post-implementation, 12/13 cases had AUS findings (92%), and no cases required surgery. Table 1 reports significant improvement in the detection of pneumatosis and portal venous gas. Of the cases with abnormal AUS findings, 5 (38%) cases had negative initial abdominal radiographs. In 5 cases (38%), AUS findings resulted in a higher Modified Bell Stage when compared to initial abdominal radiograph findings. The surgical-NEC/death rate was significantly lower following the implementation of this protocol (38% to 7%, p = 0.035) with an overall 80% decrease in surgery or death overall in infants diagnosed with NEC.
Conclusion(s): The frequency of all NEC-specific findings during AUS increased significantly, specifically in detecting pneumatosis intestinalis and portal venous gas. The surgical NEC rate is currently 7.7% (previously 38%-41%) in our Level IV NICU. AUS remains promising for adjunct use in the initial diagnostic evaluation of NEC.