Neonatology
Session: Neonatal Follow-up 1
499 - Coached, Coordinated, Enhanced Neonatal Transition (CCENT): a randomized control trial of transition to home support for parents of high-risk infants
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 499
Publication Number: 499.1191
Publication Number: 499.1191
- KE
Kayla Esser, BASc
The Hospital for Sick Children
Toronto, Ontario, Canada 
Angie Lim, RN, PhD (she/her/hers)
Post Doctoral Fellow
SickKids Hospital
Toronto, Ontario, Canada
Co-Author(s)
Presenting Author(s)
Background: Having an infant admitted to the neonatal intensive care unit (NICU) is associated with increased parental anxiety, stress and depression. These emotions may be heightened during the transition from hospital to home. Enhanced support for parents may decrease stress and improve subsequent parent and child outcomes. The Coached, Coordinated, Enhanced Neonatal Transition (CCENT) program is a novel bundled intervention for parents of high-risk infants delivered by a nurse navigator who provides 1) coaching and psychosocial support within an Acceptance and Commitment Therapy (ACT) framework, 2) care coordination, and 3) anticipatory education around the care for a medically complex infant.
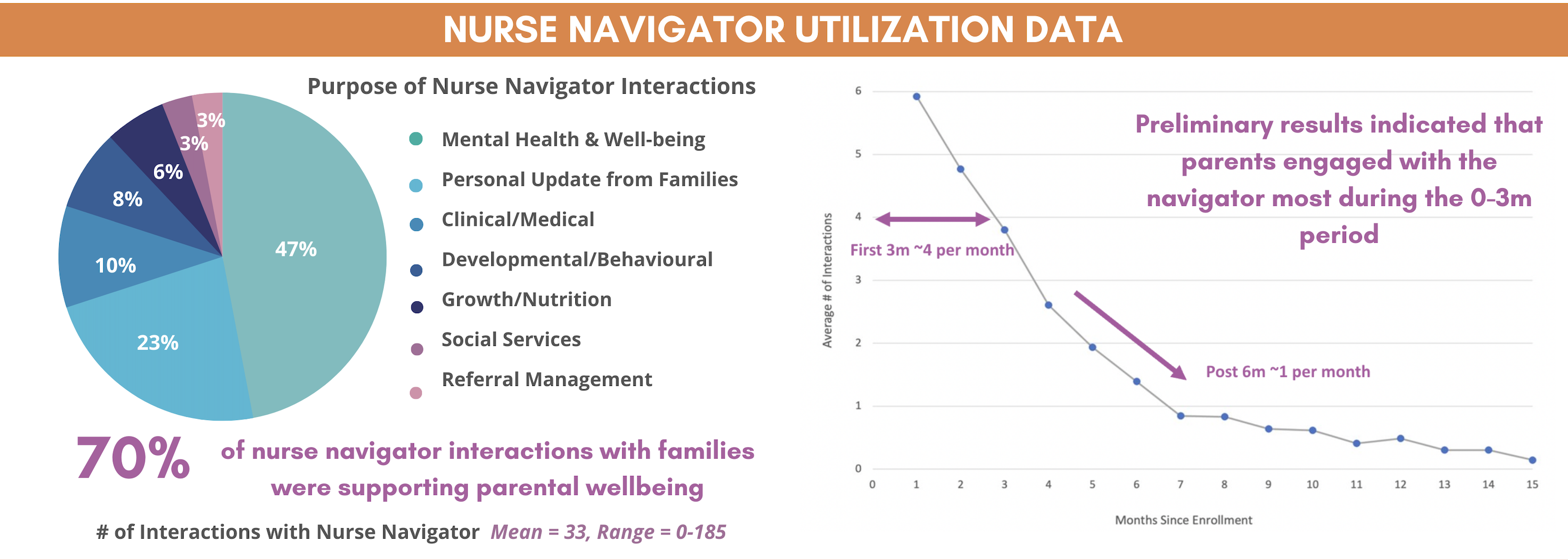
Objective: To quantitatively and qualitatively evaluate the novel role of the nurse navigator, including reasons parents engaged with the nurse navigator, the frequency, method and duration of interactions, and relationships with the nurse navigator.
Design/Methods: This is a multi-centre randomized controlled trial with 1:1 allocation to the CCENT intervention versus standard of care. Parents of high-risk infants were recruited from 7 NICUs across Canada. Participants randomized to the intervention were assigned a nurse navigator who provided the bundled intervention for 12 months. Outcomes were measured at five time points, including intervention engagement and parenting stress. Qualitative interviews were conducted to explore parent perspectives on the intervention.
Results: A total of 275 parents of high-risk infants participated in the study. Of the 138 in the intervention group, 90% of participants engaged with the nurse navigator more than 10 times throughout the year (mean interactions = 30, range = 0-185) and 88% attended at least 1 ACT session (mean attendance = 2.8 ACT sessions, range = 0-4). The majority (70%) of interactions focused on parental mental health and well-being. Parenting stress was not significantly different between intervention and control at 12 months. Four themes were identified from the qualitative interviews: the role of the nurse navigator in supporting wellbeing, the importance of having someone who understands the NICU experience, parents use of ACT and mindfulness, and parent stress during the NICU admission and first year of life.
Conclusion(s): The novel role of a nurse navigator in the NICU can enhance support for parents during and after their infant’s hospital admission. Elements of the CCENT intervention and nurse navigator role may be adapted and embedded into NICU and neonatal follow-up teams in order to provide a softer transition to home for parents of high-risk infants.