Adolescent Medicine
Session: Adolescent Medicine 1
150 - In-Person vs. Virtual Adolescent Eating Disorder Care: Demographic, Clinical and Outcome Data
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 150
Publication Number: 150.517
Publication Number: 150.517

Gail D. Gutman, MD (she/her/hers)
Fellow
Cohen Children's Medical Center
New York, New York, United States
Presenting Author(s)
Background: The Covid-19 Pandemic and lockdown measures increased the use of telemedicine worldwide. Among adolescent medicine physicians who treat eating disorders (EDs), many incorporated telemedicine into their regular practice. Little is known of the impact of telemedicine on eating disorder care.
Objective: This study seeks to compare the demographic and clinical characteristics and outcomes of adolescent patients with EDs that were seen in our division during the pandemic in-person versus virtually.
Design/Methods: We studied demographic and clinical characteristics and outcomes in patients (ages 7-21 years old) that presented to our division with EDs from September 1, 2020 to May 31, 2021. These patients were categorized as seen in-person or by telemedicine. The results were compared.
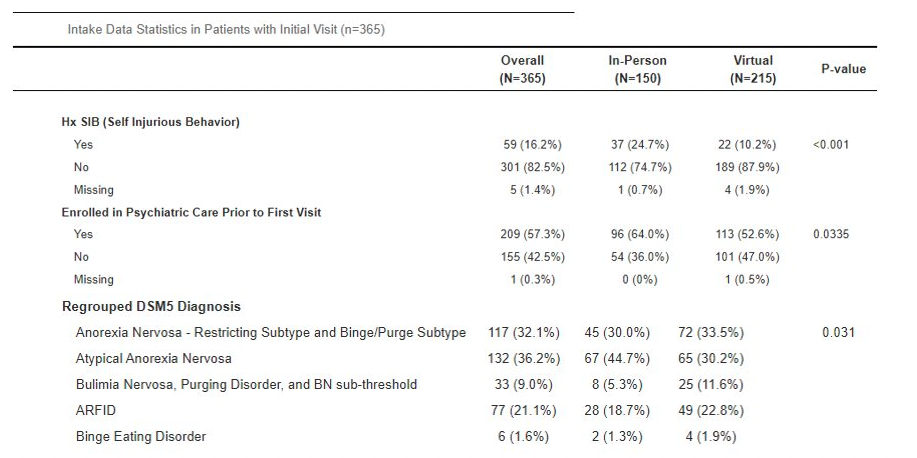
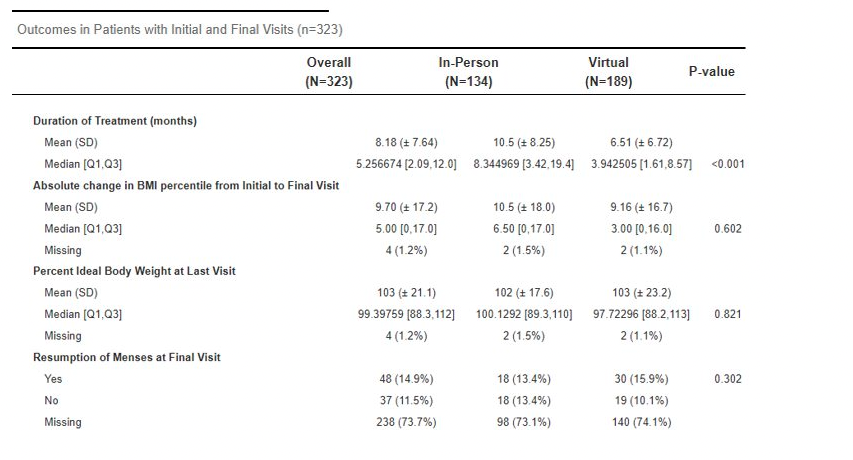
Results: Over 9 months, 365 patients presented for an initial ED visit—150 in the In-Person Group (IPG) and 215 in the Virtual Group (VG). There were no significant differences in illness severity on presentation or discharge from clinic between the two groups. There were differences in the psychiatric history and diagnosis: 24.7% of patients in IPG had history of self injurious behavior (SIB) compared to 10.2% of VG (p < 0.001). 64.0% of IPG had prior psychiatric care compared to 52.6% of VG (p=0.0335). 44.7% of IPG were diagnosed with atypical anorexia nervosa (AAN) compared to 30.2% of VG (p=0.031). Additionally, treatment length was different: Patients in VG were treated for 6.51 months compared to 10.5 months in IPG (p < 0.001) despite no significant differences in clinical outcome (eg. change in BMI, percent of ideal body weight, resumption of menses).
Conclusion(s): Among our adolescent patients treated for eating disorders by telemedicine or in-person visits, there were no differences in most clinical variables. Interestingly, patients seen virtually were in treatment for 4 months less than those in person. Several variables could explain this. First, the patients in IPG were more psychiatrically ill, with more SIB and psychiatric care. This may have influenced the social worker screening the patients, as well as their parents, to choose an in-person visit for these patients. Similarly, the psychiatric complexity may have necessitated longer treatment. The difference in treatment length may also be due to patients seeing different physicians. Further studies are needed to assess in-person versus telemedicine treatment. Nonetheless, it is shown that ED patients seen by telemedicine had very similar presentations and outcomes as those seen in-person.