Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 2
378 - Implementation of Anxiety Screening Workflow for 8-18-Year-Old Patients: A Resident-Led QI Project
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 378
Publication Number: 378.2121
Publication Number: 378.2121

Marisa E. Boch, MD (she/her/hers)
Resident Physician
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: The American Academy of Pediatrics (AAP) and United States Preventive Services Task Force (USPSTF) established new recommendations in 2022 for routine anxiety screening among children ages 8-18 in response to rising rates of childhood anxiety. There is a lack of literature on standardized anxiety screening workflows, particularly in residency-affiliated clinics. We initiated a quality improvement (QI) project to incorporate anxiety screening into standard practice, in accordance with the new guidelines.
Objective: Our primary aim was to implement standardized anxiety screening in at least 50% of well child visits for patients ages 8-18 by April 2023. We also aimed to appropriately manage 50% of those with positive screens in accordance with a standardized workflow.
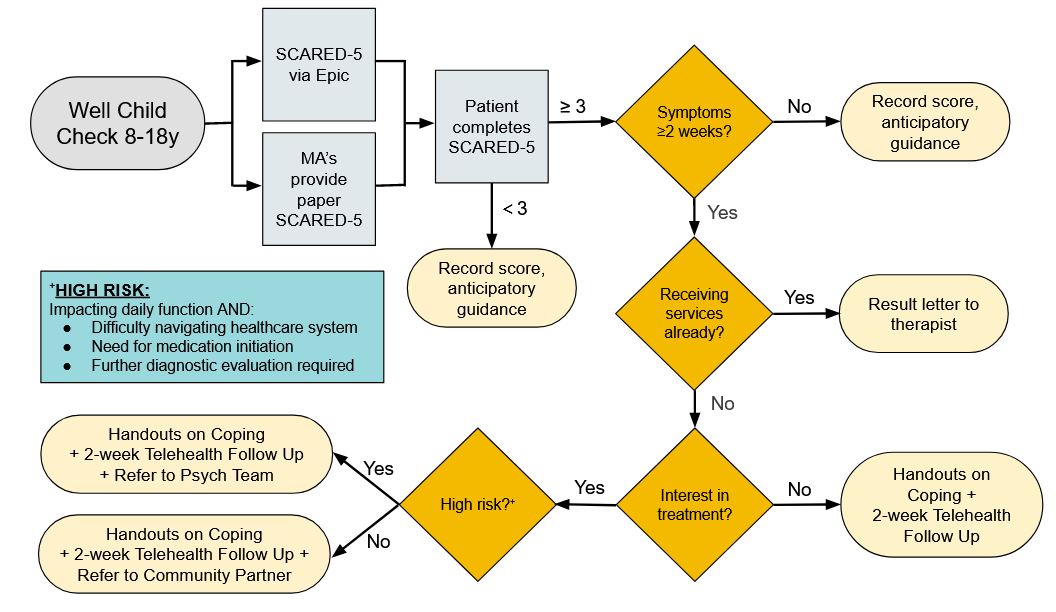
Design/Methods: This project was conducted at a residency-affiliated, community-based pediatric primary care practice in upper Manhattan. A key driver diagram (Figure 1) was created with input from a multidisciplinary team of pediatricians, mental health professionals, and practice staff. The Screen for Child Anxiety Related Emotional Disorders scale was chosen for its validated use in children and was given to eligible patients at the beginning of well child visits. The workflow for screening and management was then conducted with PDSA cycles derived from key drivers to 1) improve provider and staff knowledge, 2) standardize workflow, 3) adapt screeners, 4) streamline disposition, and 5) align community resources.
Results: The anxiety screening rate increased from 0% to a maximum 81.8% over 9 months of implementation and remained above goal after project completion, as denoted in the run chart (Figure 2). PDSA cycle interventions, including provider email reminders, updated Epic smartphrases, and provider performance reports, were successful tools to increase screening rates as evidenced by the shifting median line. Screening rates were significantly higher for patients ages 12-18 compared to ages 8-11 (p < 0.05) but did not significantly differ by gender, language, or provider type. Of patients who screened positive, >75% were managed correctly according to the developed workflow (Figure 3), with >70% managed without community referral.
Conclusion(s): This QI project implemented a standardized and sustainable anxiety screening that adheres to new AAP and USPSTF guidelines. It also created a management workflow that ensures support for patients with anxiety without significantly burdening community mental health resources. This project may serve as a model for other primary care practices to implement sustainable anxiety screening workflows.
.jpg)
.jpg)
