Neonatology
Session: Neonatal General 2: NICU Care Strategies
76 - Impact of Transfer of Care at Greater than 20 Weeks Gestation on Maternal and Neonatal Outcomes
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 76
Publication Number: 76.164
Publication Number: 76.164

Caitlin Gonsolin, MD (she/her/hers)
Neonatology Fellow
Brooke Army Medical Center
Schertz, Texas, United States
Presenting Author(s)
Background: The impact of mid-late pregnancy transfer of care (TOC) on maternal and neonatal outcomes is currently unknown. There are limited studies illustrating that maternal stress is associated with both preterm birth and low birth weight, but no data on more robust neonatal and maternal outcomes. To strive for constantly improving healthcare, it is crucial to understand the implications of TOC during pregnancy.
Objective: Study
Aims: (1) Determine the incidence and timing of TOC at greater than 20-weeks gestation within a single military treatment facility. (2) Compare the rate of adverse maternal and neonatal outcomes to baseline data. (3) Explore the experience of mothers who underwent TOC.
Design/Methods: Explanatory sequential mixed methods design was utilized, with a retrospective cohort review of pregnant individuals who had transferred care at >20 weeks and had live births between Jan 2017-Dec 2021. Descriptive statistics were applied to report maternal and neonatal variables/outcomes. Local data from one calendar year (2018) was used for baseline comparison and statistical analysis was conducted using a Pearson’s Chi Square analysis. Interviews were conducted with nine women who underwent TOC, detailing their experience, with descriptive thematic analysis performed on interview transcripts.
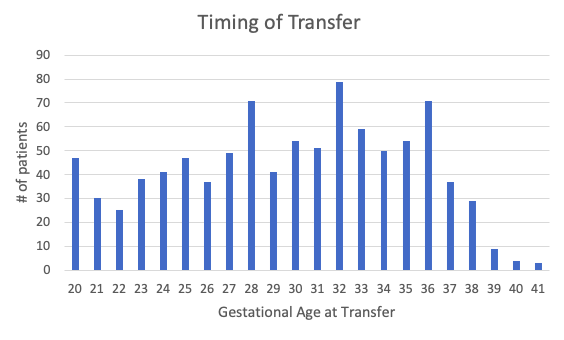
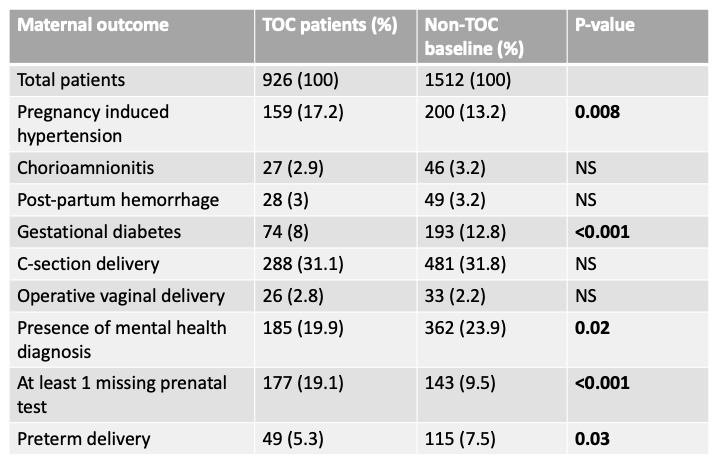
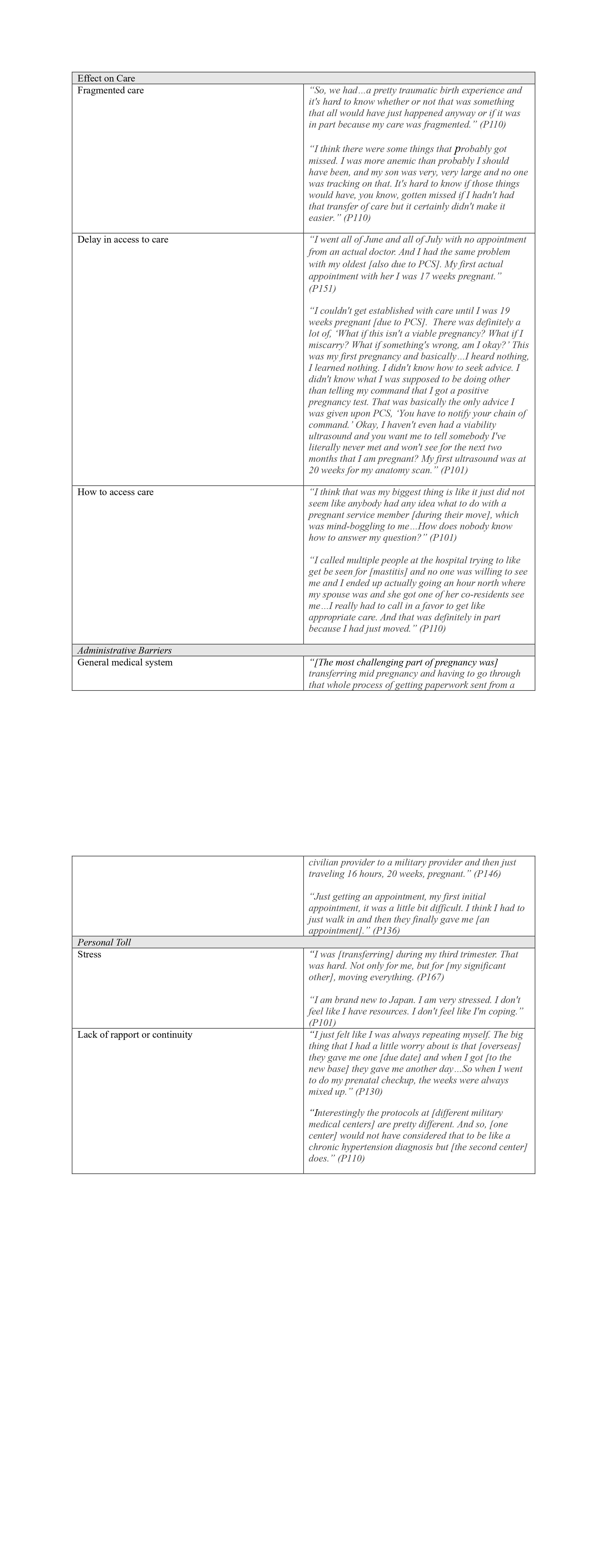
Results: There were 926 individuals who transferred care at >20 weeks, with 939 live births. Median age at transfer was 30 weeks (Figure 1). Twenty patients transferred care within a week of delivery. Maternal outcomes for those who transferred care vs. baseline rates from 2018 at the same center are presented in Table 1. Infants delivered at a mean gestational age of 38.8 weeks and birthweight of 3332 grams. Nearly 14 percent (13.6%) of infants underwent sepsis evaluation with antibiotic coverage. Ninety-seven neonates (10.3%) required NICU admission with an average length of stay of 2.7 days. Thematic analysis revealed several impacts to mothers who experienced TOC (Table 2).
Conclusion(s): Mid-late pregnancy TOC is a common occurrence for military affiliated women. This single-center study revealed some significant differences between mid-late pregnancy TOC and baseline data, some of which may reflect a lapse in access to care rather than true differences in patient populations. Qualitative analysis revealed a significant burden for pregnant mothers who undergo TOC. Further examination of maternal and neonatal outcomes, as well as the maternal experience following TOC across the military health system is crucial to better ensure optimal provision of care for this population.