Asthma
Session: Asthma 1
193 - Identifying Barriers to Implementation of Guidelines Based Asthma Care
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 193
Publication Number: 193.525
Publication Number: 193.525
- JS
Jessica Stern, MD MS (she/her/hers/ella)
Associate Professor
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Presenting Author(s)
Background: Asthma is the most prevalent chronic condition of childhood, affecting 9 million children in the US. Up to 80% of people with asthma have comorbid allergic rhinitis; yet allergic rhinitis is often under-recognized and undertreated especially in Black and Latinx children. To reduce disparities in asthma outcomes there is a need to address the gap in recognition and treatment of allergic rhinitis in children with asthma as recommended by the NHLBI guidelines.
Objective: The goal of this research was to assess clinician and family barriers to recognition and treatment of allergic rhinitis among school children with asthma. We hypothesized that modifiable barriers exist in screening for, identifying, and appropriately treating co-morbid allergic rhinitis in children with persistent asthma.
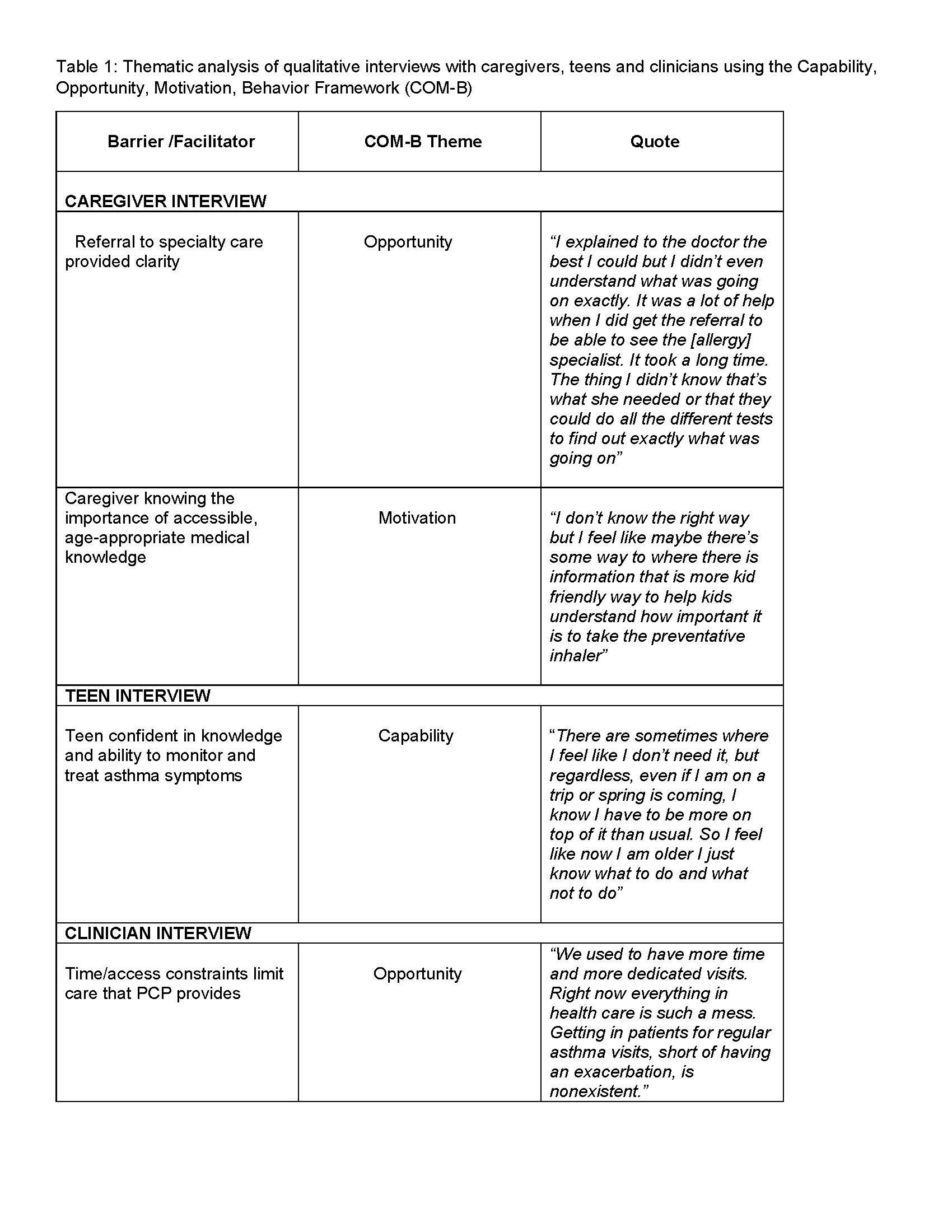
Design/Methods: We conducted semi-structured interviews using the COM-B model and the Theoretical Domains Framework. Interviews assessed barriers and facilitators to screening, recognizing, and treating co-morbid allergic rhinitis in children with asthma. Participants included pediatric primary care physicians (N=9; avg. years in practice:15), as well as adolescents (N=13; mean age 13.6 yrs., 53% Black, 31% Latinx) and caregivers (N=20; 43% Black, 30% Latinx), who had recently completed a school-based asthma trial. Qualitative analysis was driven by a thematic approach.
Results: The data suggest barriers to guideline-based care, especially assessment and treatment of allergic co-morbidities among children with persistent asthma. Barriers to environmental assessment, referral to specialty care, and knowledge of the guidelines are emerging themes (Table 1). Specifically, physicians noted competing priorities as a barrier to guideline - based asthma care, while caregivers noted specialty care facilitating improved understanding of allergic disease and asthma, and also highlighted the need to tailor information in a way that is accessible to adolescents. Adolescents noted increased capability in managing their chronic disease.
Conclusion(s): Persistent and pervasive disparities exist among Black and Latinx children with asthma despite evidence-based guideline recommendations. Leveraging implementation science to understand barriers to guideline-based care can proactively guide interventions to close these gaps. These findings will be used to develop assessment and treatment tools/pathways with the goal of reducing disparities in asthma outcomes.