Emergency Medicine
Session: Emergency Medicine 9: Respiratory
229 - A Retrospective Study of Trends in Testing and Treatment for Viral Lower Respiratory Tract Infection in Young Children Following the COVID-19 Pandemic
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 229
Publication Number: 229.3323
Publication Number: 229.3323

Emily J. Labudde, MD (she/her/hers)
Resident Physician
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: In the last 20 years, rates of low-value care (ineffective, unnecessary, or wasteful practices) have steadily decreased for children with bronchiolitis. The effects of the COVID-19 pandemic and 2022 winter “tridemic” on rates of low-value care, however, have not been studied.
Objective: We sought to determine whether rates of low-value care in young children with bronchiolitis increased nationally following the COVID-19 pandemic.
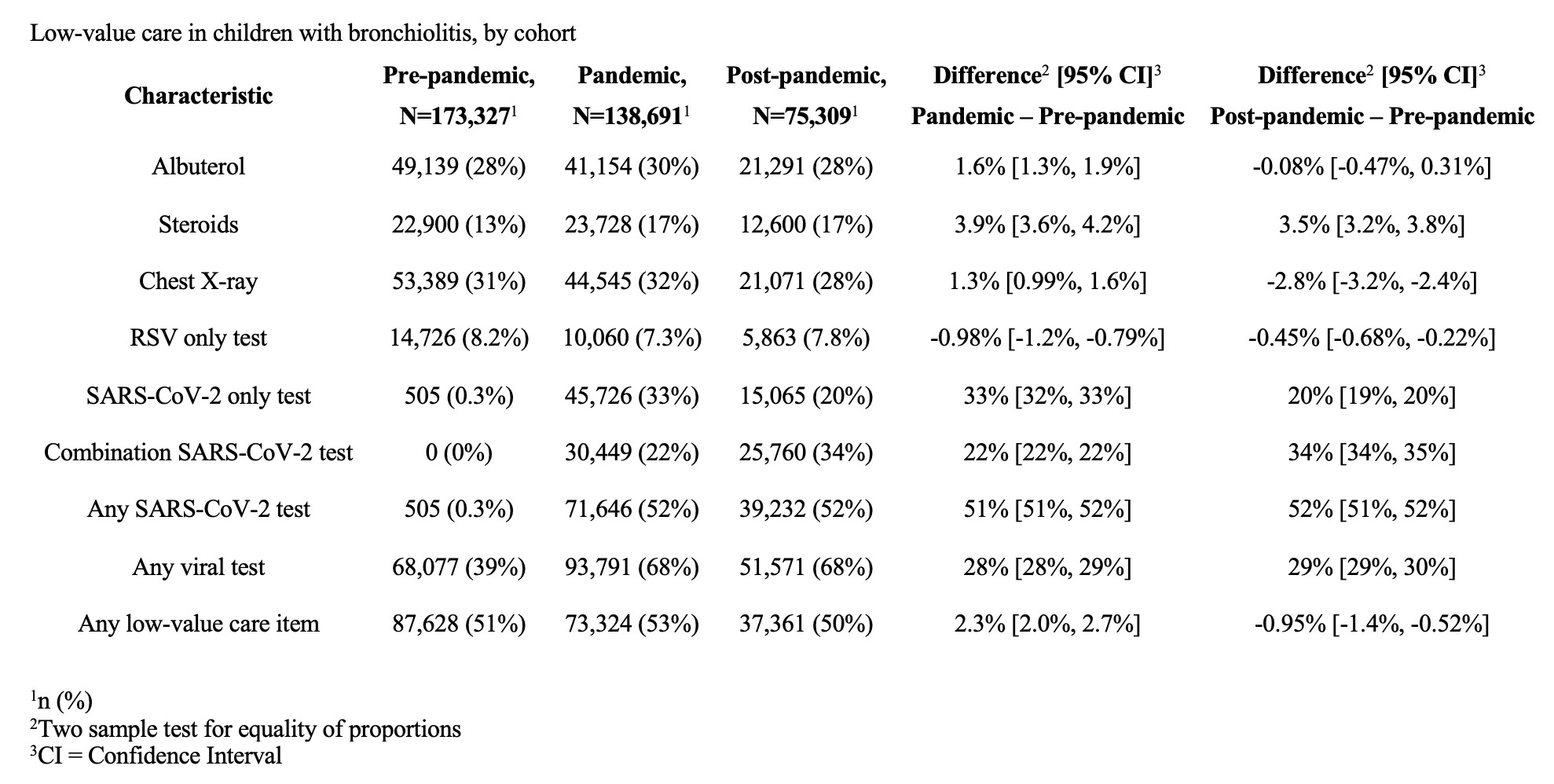
Design/Methods: This was a retrospective study of the Pediatric Health Information Systems (PHIS) database including children < 2 years of age seen in a pediatric emergency department for bronchiolitis. We selected a priori September 1, 2018, to February 28, 2020 (pre-pandemic), March 1, 2020 to August 31, 2022 (pandemic), and September 1, 2022 to January 31, 2023 (post-pandemic) as the 3 study periods. Low-value care was the main study outcome and included viral testing, chest radiography, albuterol, and corticosteroids. We compared the percentage of patients with any and each low-value care element across the 3 time periods [main measure % difference and 95% confidence interval (CI)].
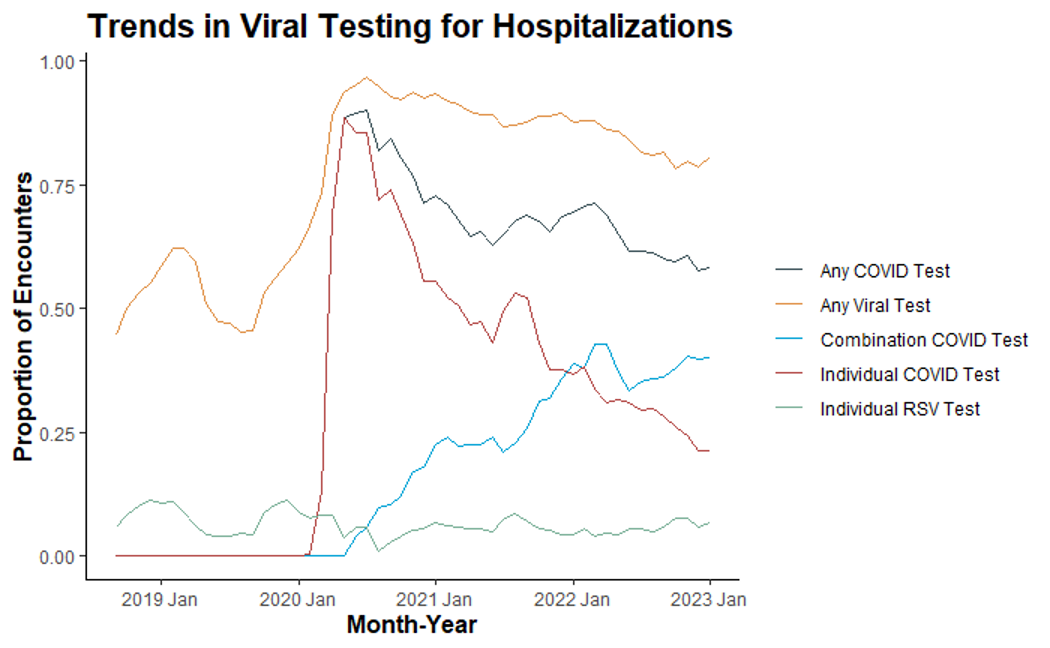
Results: We included 387,478 encounters: 173,478 (45%) pre-pandemic, 138,691 (36%) pandemic, and 75,309 (19%) post-pandemic. The percentage of patients with any low value care was 51%, 53%, and 50% across the 3 periods, respectively. There was little variation in the use of albuterol (28-30%), chest radiography (28-32%), and RSV testing (8%; 95% CI for nearly all differences inclusive of 0). Systemic steroid use was 13% pre-pandemic and 17% in both pandemic and post-pandemic periods (+3.5%, 95% CI 3.2-3.8%). Viral testing was performed in 39% pre-pandemic and 68% in both pandemic and post-pandemic periods (+29%, 95% CI 29-30%). The increase in viral testing appeared to be driven by testing for SARS-CoV-2 (52% of encounters in both pandemic and post-pandemic periods). Combination testing, including SARS-CoV-2 and at least one other virus, increased from 22% in the pandemic period to 34% in the post-pandemic period, while single virus testing for SARS-CoV-2 decreased from 33% to 20% respectively.
Conclusion(s): Despite increased volumes of patients with bronchiolitis during the fall and winter of 2022, there was no major increase in the use of low-value care. Due to SARS-CoV-2 testing, overall rates of viral testing increased dramatically over time; however, viral testing remained high even when COVID-19 incidence declined. Future bronchiolitis guidelines should consider updating viral testing recommendations to account for the rise in combination viral testing.
.png)
