Adolescent Medicine
Session: Adolescent Medicine 1
137 - Gender Diverse Goals and Outcomes in a University Health Setting
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 137
Publication Number: 137.31
Publication Number: 137.31

Stephanie M. Hartman, MD (she/her/hers)
Associate Director of Primary Care
University of Virginia Student Health and Wellness
Charlottesville, Virginia, United States
Presenting Author(s)
Background: Visits for gender diverse (GD) care have increased at many university health centers and care for gender diverse patients by primary care providers at university health centers represents an evolving area of clinical practice. This study was conducted at a large, public university student health center with a gender diverse care team to determine best gender diverse medical care for the university-aged population.
Objective: The objective of this study was to understand gender affirmation goals and outcomes of university students including hormone replacement therapy (HRT) and gender-affirming procedures.
Design/Methods: GD patients were identified from ICD-10 codes (F64.0, F64.8, F64.9, Z79.899, Z87.890) pertaining to gender dysphoria who had a specific visit for GD care. Retrospective chart review was performed to collect data on GD visits between August 2017 and June 2023. Data included: gender identity, initial transition goals, HRT, medical procedures, and achievement of goals. This study was approved by the University IRB.
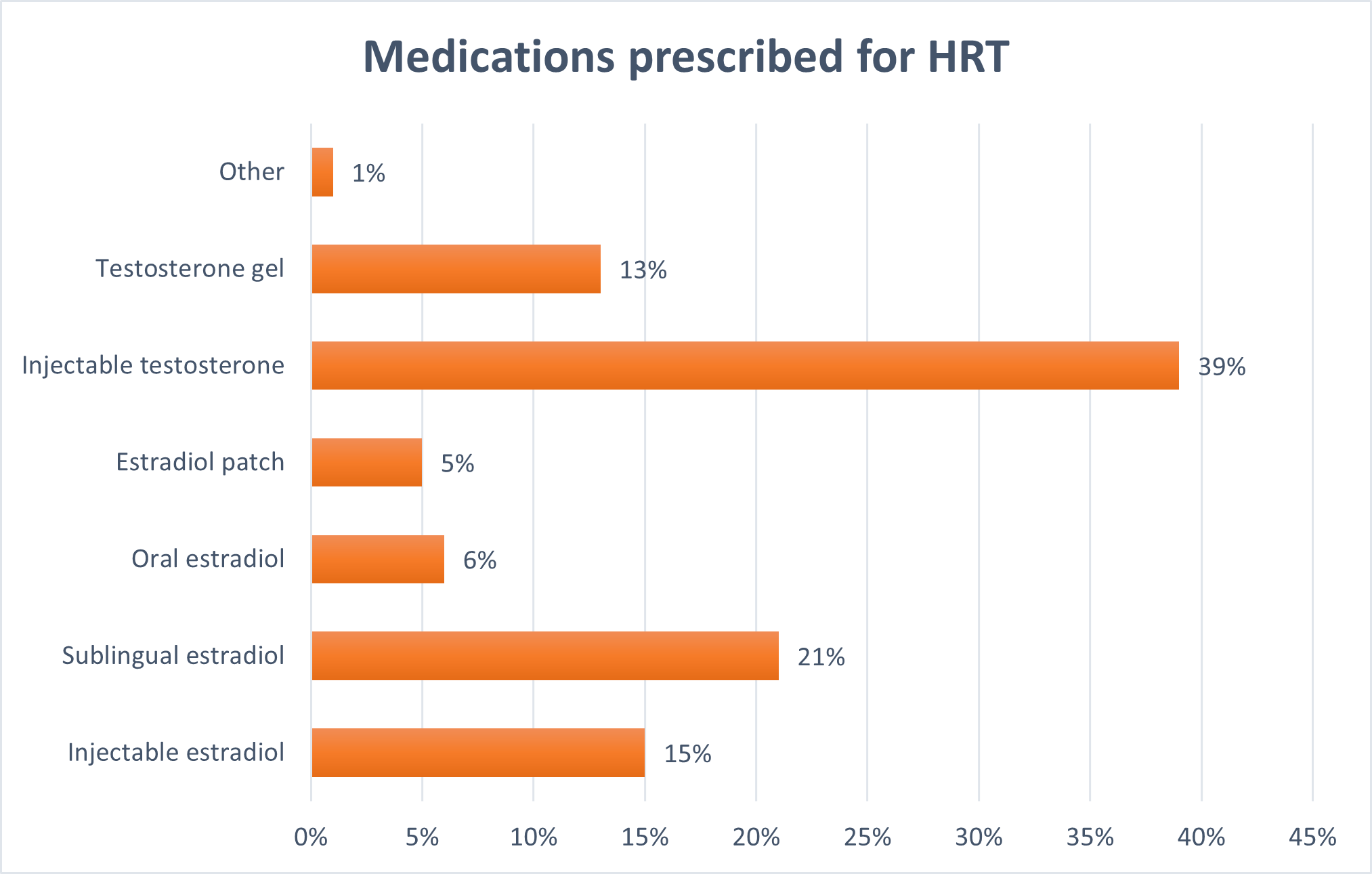
Results: During the study period, there were 121 GD patients with an initial GD visit. These patients self-identified as transfemale (32.2%), transmale (27.3%), non-binary or genderqueer (31.4%), male (1.7%) and uncertain/still exploring (7.4%). Transition goals included: desire to present as their gender identity (66%), proceed with medical or surgical procedures (46%), start HRT (45%), continue hormones (29%) and uncertain (13%). Of the 67% of patients who were prescribed HRT, 27% used estradiol tablets, 39% injectable testosterone, 15% injectable estradiol, 5% estradiol patch, 13% testosterone gel, and 1% other. In addition, 18% of students underwent a surgical procedure while a student at the university with 68% of them receiving top surgery. To decrease potential side effects, 86% of patients took sublingual or subcutaneous estradiol rather than oral estradiol. Of the patients who were prescribed HRT, 63% reached optimal hormone levels per published guidelines and 37% were still transitioning upon graduation or the end of the study period.
Conclusion(s): Adolescents and young adults approach gender diverse health care visits with different goals in mind. These goals can range from adjusting hormone doses to understanding other avenues for non-medical transition including presenting in gender congruent dress and other social changes.. Knowledge of personal transition goals allows providers to offer improved and patient-centered care and position patients for optimum hand-off of care to a PCP after leaving the university setting.
.png)
.png)
