Back
Background: Effective communication has routinely been shown to improve patient outcomes as well as employee satisfaction and is especially important when managing complex patients in the acute setting. The busy cardiology service at our large, quaternary care hospital experienced shifts in communication style during the COVID-19 pandemic and after the roll out of a new messaging platform, leading to increased concerns related to communication between nurses and residents. Quality improvement techniques have been utilized to improve communication in a wide array of settings, but few studies have looked at its utility in nurse and resident communication.
Objective: The goal of this longitudinal QI project was to improve nursing and resident perceptions of communication as measured by an increase in the percentage of survey respondents rating team communication as “Good” or “Very Good” from 36% for nursing and 65% for residents (baseline) to 75% for both by August 2023.
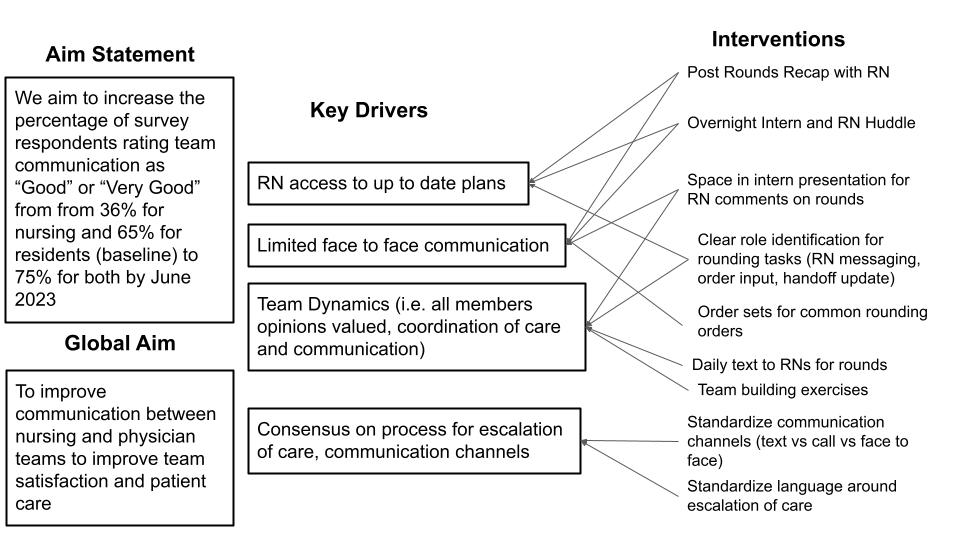
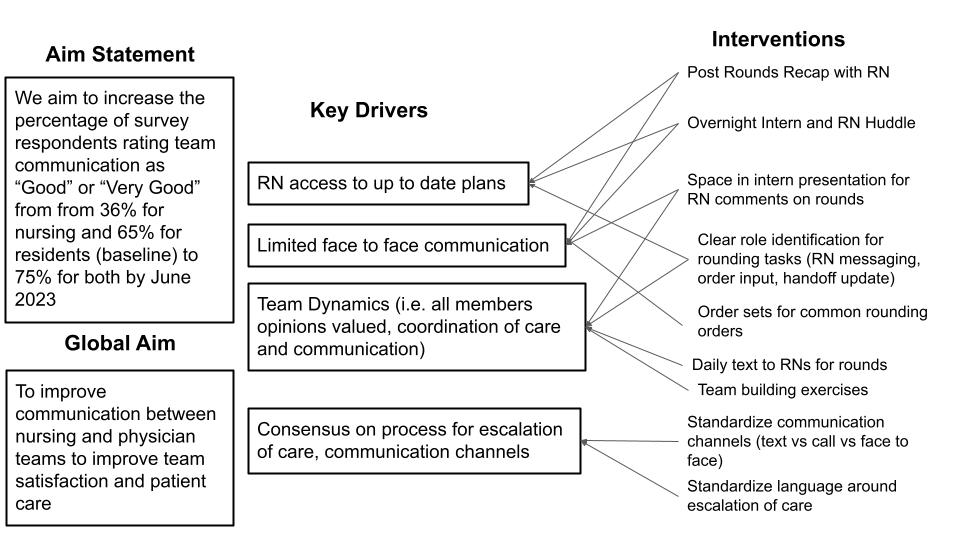
Design/Methods: A team of key stakeholders, including residents, attendings, nurses, and nursing leadership met to identify barriers to communication and areas for improvement. A survey was distributed to nurses on the cardiology floor and residents who had rotated on the cardiology team during the academic year 2022-2023. Based on identified barriers a key-driver diagram (Figure 1) was developed and the following interventions were implemented using a Plan-Do-Study-Act model: creation of a daily text chain between nurses and residents, initiation of an overnight huddle between residents and nurses, and posting reminders to call nurses to rounds on resident workstations. Perceptions of communication were assessed monthly through surveys of nurses and residents.
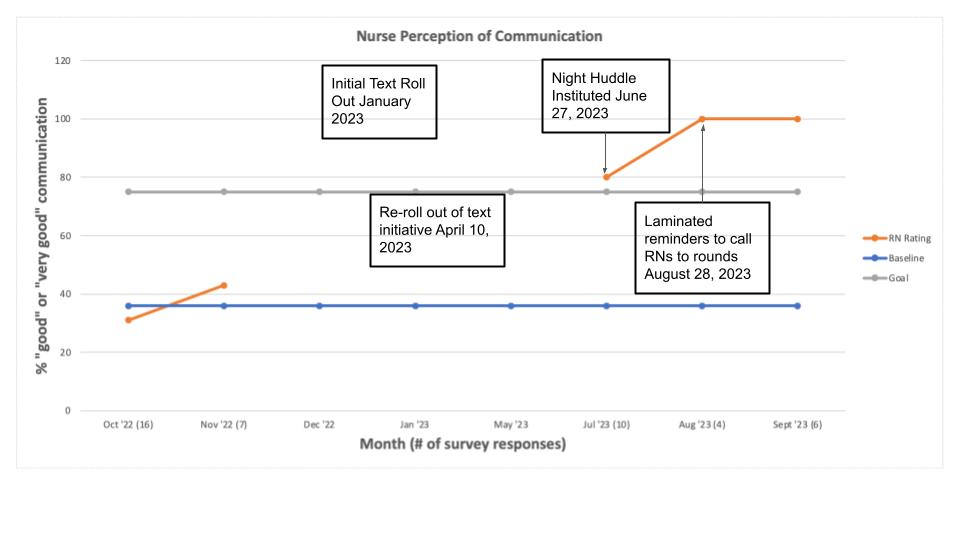
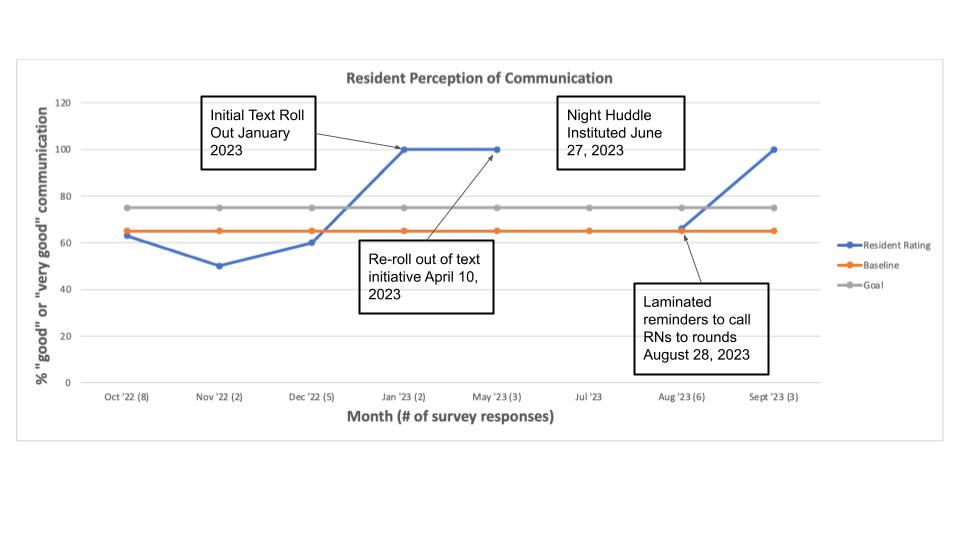
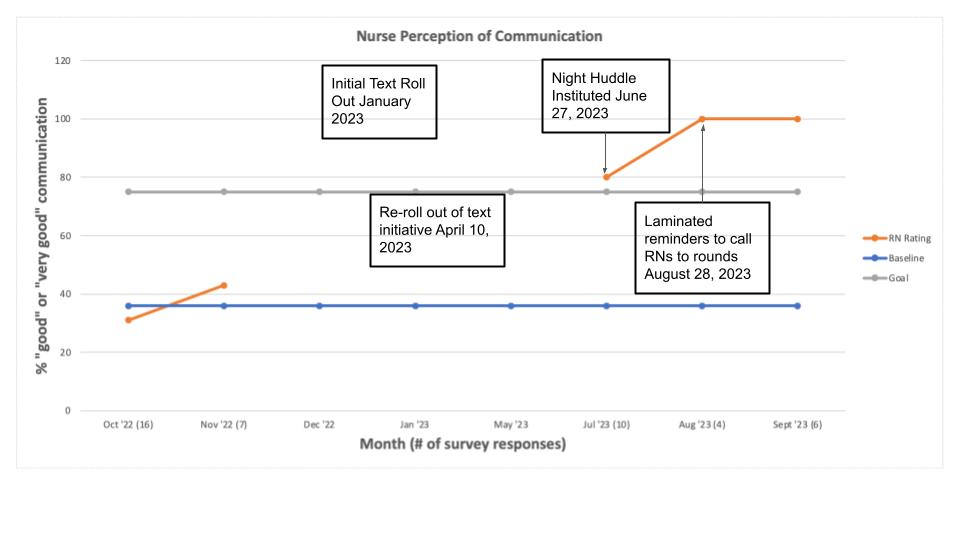
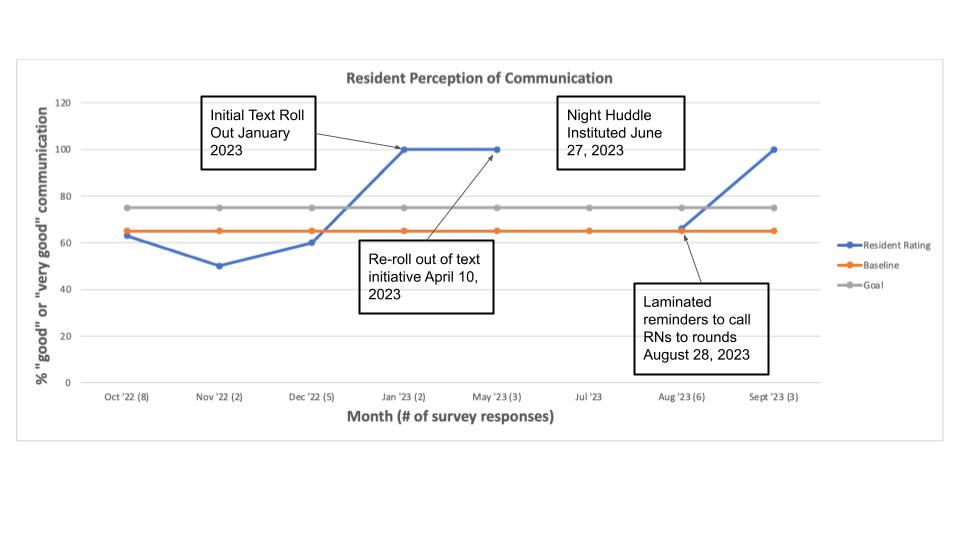
Results: Baseline data collected from October through December 2022 revealed that 36% of nurses and 65% of residents rated team communication as “Good” or “Very Good.” Between July and September nurses' perceptions of communication exceeded our goal of 75% (Figure 2) and in September residents' perceptions of communication exceeded our goal (Figure 3). There were struggles related to survey response rates in the winter and late spring of 2023 thought to be related to higher patient volumes in the winter months and survey fatigue which improved with increased outreach by nursing leadership and the resident team.
Conclusion(s): Nursing perceptions of communication were improved through targeted interventions developed by a large group of key stakeholders. Further work is needed to sustain improvement in resident perceptions of communication and to clarify communication around escalation of care.
Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
32 - A QI Approach to Improving Communication between Nurses and Residents on a General Cardiology Team
Monday, May 6, 2024
9:30 AM – 11:30 AM ET
Poster Number: 32
Publication Number: 32.3301
Publication Number: 32.3301
Sarah A. Frantz, MD (she/her/hers)
Pediatrics Resident
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Effective communication has routinely been shown to improve patient outcomes as well as employee satisfaction and is especially important when managing complex patients in the acute setting. The busy cardiology service at our large, quaternary care hospital experienced shifts in communication style during the COVID-19 pandemic and after the roll out of a new messaging platform, leading to increased concerns related to communication between nurses and residents. Quality improvement techniques have been utilized to improve communication in a wide array of settings, but few studies have looked at its utility in nurse and resident communication.
Objective: The goal of this longitudinal QI project was to improve nursing and resident perceptions of communication as measured by an increase in the percentage of survey respondents rating team communication as “Good” or “Very Good” from 36% for nursing and 65% for residents (baseline) to 75% for both by August 2023.
Design/Methods: A team of key stakeholders, including residents, attendings, nurses, and nursing leadership met to identify barriers to communication and areas for improvement. A survey was distributed to nurses on the cardiology floor and residents who had rotated on the cardiology team during the academic year 2022-2023. Based on identified barriers a key-driver diagram (Figure 1) was developed and the following interventions were implemented using a Plan-Do-Study-Act model: creation of a daily text chain between nurses and residents, initiation of an overnight huddle between residents and nurses, and posting reminders to call nurses to rounds on resident workstations. Perceptions of communication were assessed monthly through surveys of nurses and residents.
Results: Baseline data collected from October through December 2022 revealed that 36% of nurses and 65% of residents rated team communication as “Good” or “Very Good.” Between July and September nurses' perceptions of communication exceeded our goal of 75% (Figure 2) and in September residents' perceptions of communication exceeded our goal (Figure 3). There were struggles related to survey response rates in the winter and late spring of 2023 thought to be related to higher patient volumes in the winter months and survey fatigue which improved with increased outreach by nursing leadership and the resident team.
Conclusion(s): Nursing perceptions of communication were improved through targeted interventions developed by a large group of key stakeholders. Further work is needed to sustain improvement in resident perceptions of communication and to clarify communication around escalation of care.