Neonatology
Session: Neonatal Follow-up 1
487 - Parent Perspectives and Child Outcomes with Virtual Care in Neonatal Neurodevelopmental Follow-up Clinic: A Mixed Methods Study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 487
Publication Number: 487.1639
Publication Number: 487.1639
- KR
Kamini Raghuram, MD (she/her/hers)
Staff Neonatologist; Director, Neonatal Neurodevelopmental Follow-up Clinic
Mount Sinai Hospital
Toronto, Ontario, Canada
Presenting Author(s)
Background: The SARS-CoV-2 pandemic accelerated the use of virtual care in neonatal neurodevelopmental follow-up (NNFU) clinic. However, this transition was abrupt with limited information to guide its use effectively. In particular, parent perspectives on virtual care and its impact on developmental outcomes has not been evaluated systematically.
Objective: The objectives of this study are to (1) qualitatively evaluate parents’ and healthcare professionals’ experiences with virtual care in the NNFU context and (2) quantitatively assess outcomes of preterm neonates < 37 weeks GA in the era of virtual care compared to those seen in-person prior to its implementation.
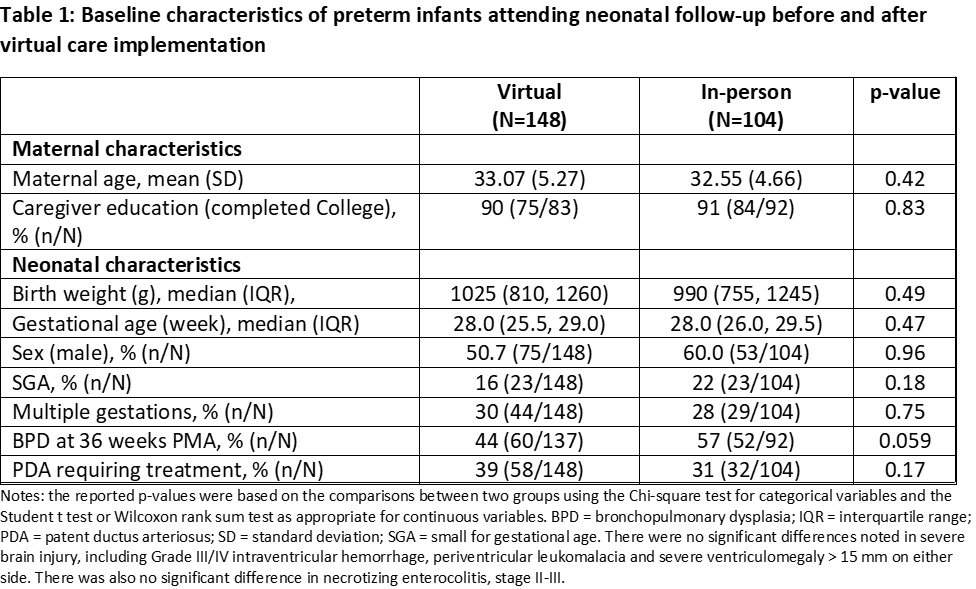
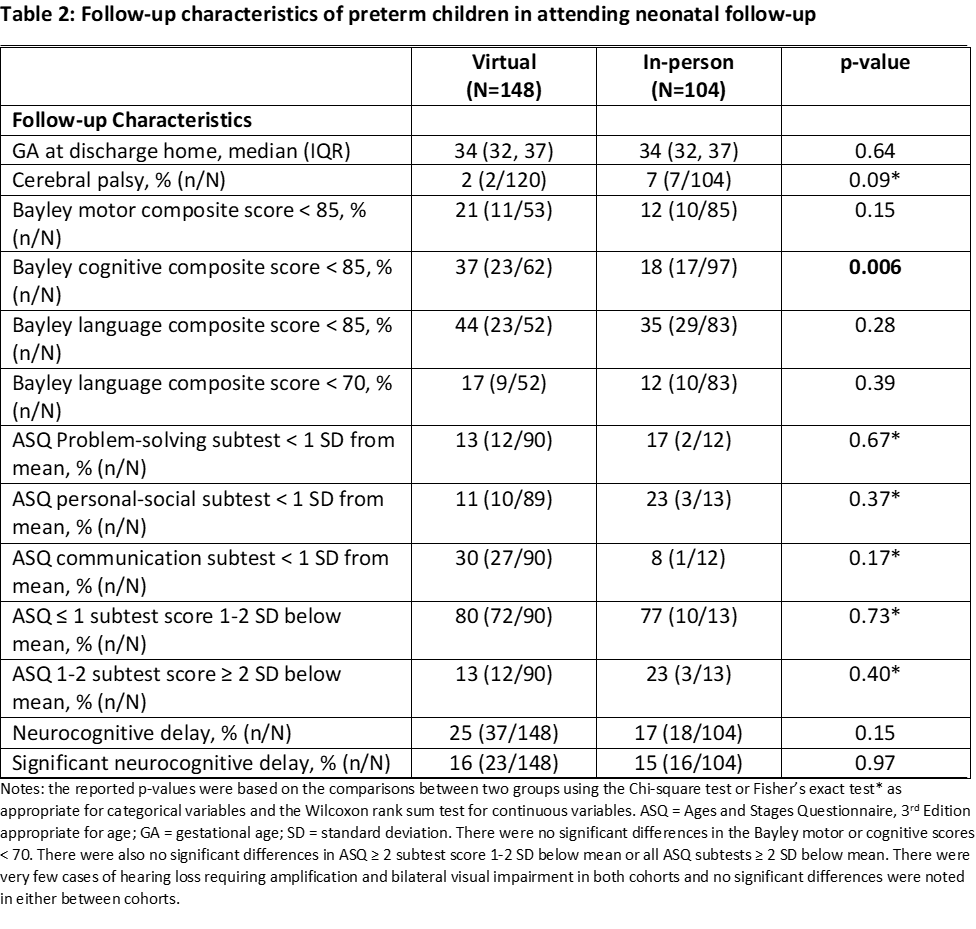
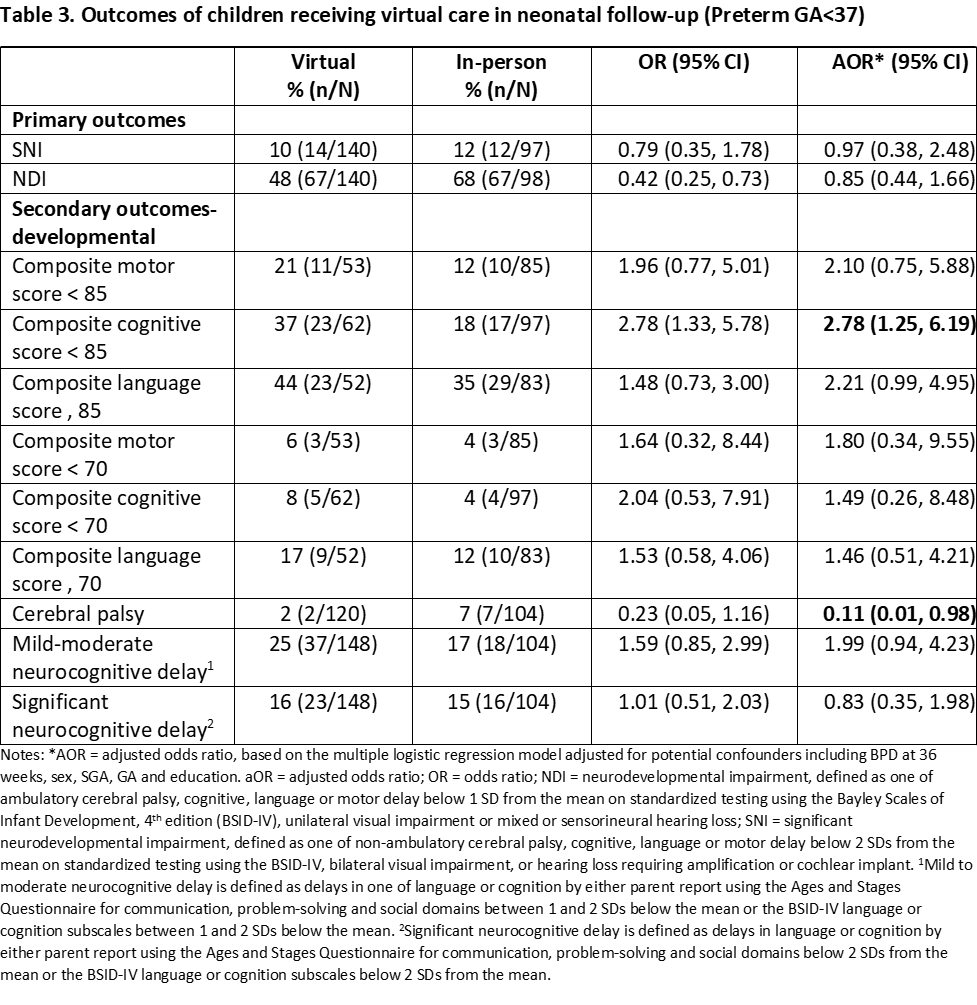
Design/Methods: Semi-structured interviews were conducted with families of high-risk infants who had attended at least two appointments at the NNFU clinic at a single tertiary hospital and thematic analysis was conducted. Neurodevelopmental outcomes of two cohorts, one that never experienced virtual care (“in-person” group) and the other who did (“virtual” group), were collected for preterm infants. Baseline characteristics and neurodevelopmental outcomes, including parent-reported problem-solving, personal-social, communication and motor skills and standardized testing for cognition, language and motor skills using the Bayley Scales of Infant Development were compared using descriptive statistics and multivariable regression modeling, respectively.
Results: Three main themes were identified: increased confidence in in-person assessments, adequate delivery of information using virtual platforms when in-person is not available and a strong preference for individualized care that ensures continuity. Baseline characteristics and neonatal morbidities were not statistically significant different between the two groups (p > 0.05). (Table 1). The incidence of cerebral palsy in the virtual group was 2% compared to 7% in the in-person group (p = 0.09), reflective of challenges in detecting motor impairment in a virtual setting (Table 2). There was no difference in the adjusted odds of mild to moderate or significant cognitive or language delay between groups (Table 3). However, standardized testing seemed to show higher odds of cognitive delay in the virtual group compared to parent-reported measures, likely reflecting the limitations of parent-reported measures in detecting subtle cognitive differences.
Conclusion(s): Parents and healthcare providers alike prefer the use of in-person assessments to provide comprehensive developmental support for families. Virtual care may be limited in detecting motor impairments, but may allow for access to information.