Neonatology
Session: Neonatal Pulmonology - Clinical Science 2: Lung Imaging, Lung Function
199 - Lung Ultrasound to predict Extubation Failure in Preterm Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 199
Publication Number: 199.3280
Publication Number: 199.3280

Arun Sett, MBBS (Hons) (he/him/his)
Neonatal Research Fellow
The Royal Women's Hospital
Melbourne, Victoria, Australia
Presenting Author(s)
Background: As mechanical ventilation is associated with respiratory morbidity in infants born < 32 weeks’ gestation, clinicians aim to expedite extubation to non-invasive respiratory support. However many very preterm infants require reintubation. The overall accuracy of predictors of extubation readiness, determined in small studies, is variable (AUCs 0.61-0.94). Many of these tests are not currently used in clinical practice. Lung ultrasound (LUS) is being increasingly used and is readily available, and may be a useful tool to determine extubation readiness.
Objective: To determine the accuracy of LUS performed pre-extubation to predict reintubation in very preterm infants.
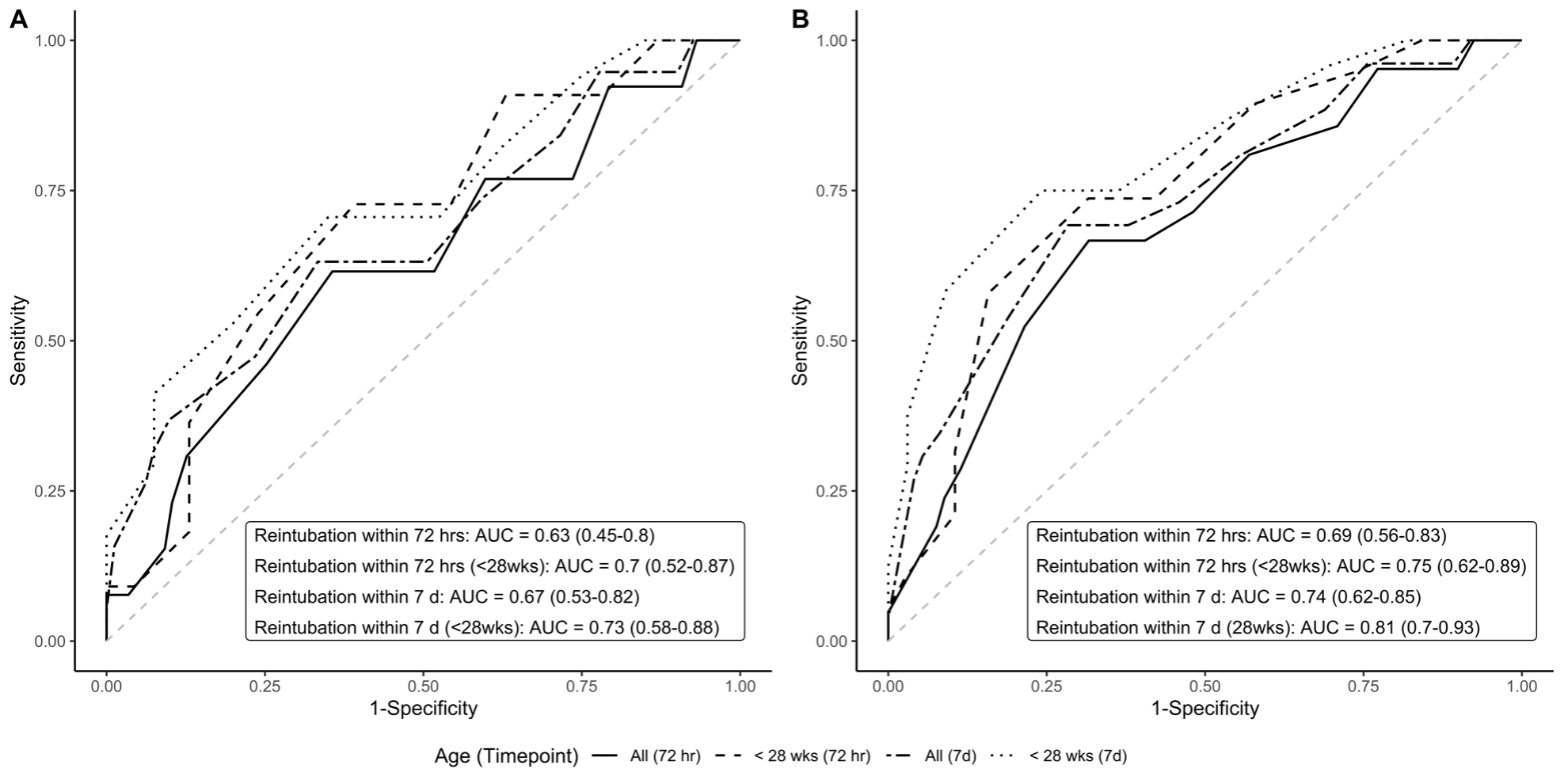
Design/Methods: Anterior and lateral LUS images were obtained before extubation. The primary outcome was the accuracy of LUS scores (score range 0-24) to predict reintubation within 72 hours. Prespecified secondary outcomes were accuracy in predicting: 1. reintubation within 7 days; 2. pre-defined clinical failure criteria at 72 hours and 7 days; and 3. reintubation and clinical failure criteria in extremely preterm infants born < 28 weeks’ gestation. Accuracy of lateral imaging only (score range 0-12) was also determined. Area under the curves (AUCs), cut-off scores, sensitivities and specificities were calculated using receiver operator characteristic (ROC) analysis.
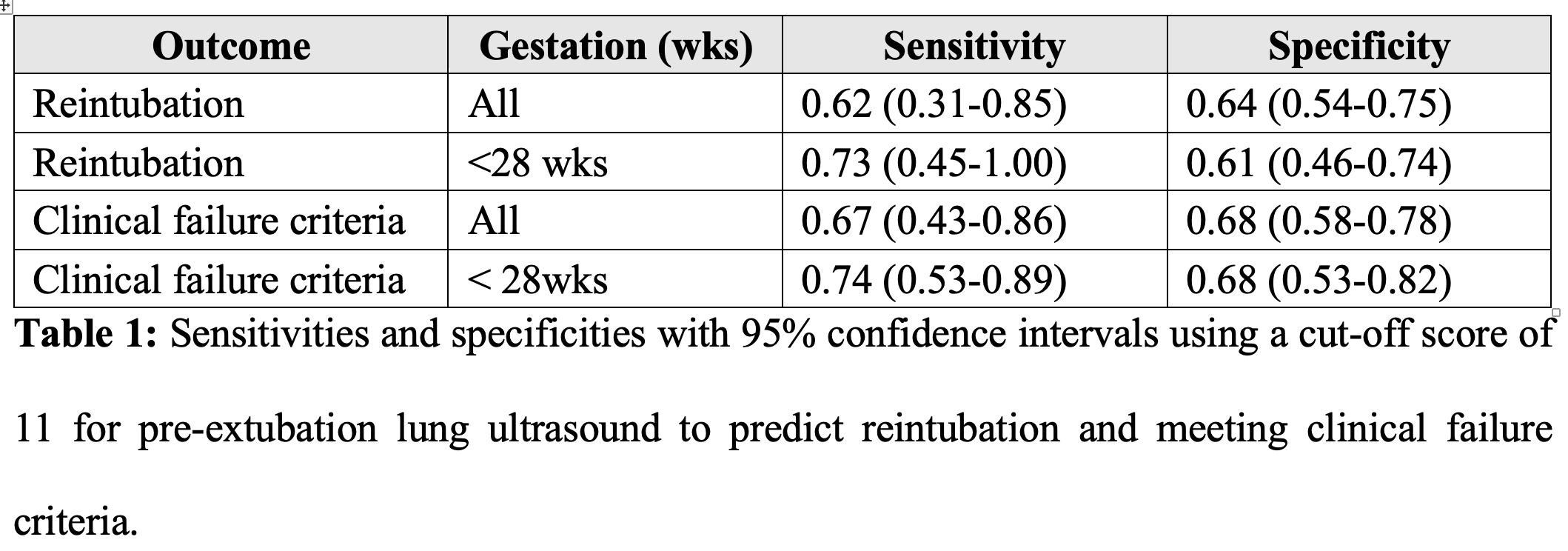
Results: One-hundred infants with a mean (SD) gestation of 27.4 (2.2) weeks and mean (SD) birthweight of 1059 (354) grams were studied. Nineteen infants (19%) were reintubated and 26 (26%) met clinical failure criteria within 72 hours. AUCs (95% CI) were 0.63 (0.45-0.80) for reintubation, and 0.69 (0.56-0.83) for meeting clinical failure criteria. Accuracy was greater in extremely preterm infants (n=57, mean [SD] gestation 26 [1.4] weeks and mean [SD] birth weight; 875 [190] grams ) with respective AUCs of 0.70 (0.52-0.87) for reintubation, and 0.75 (0.62-0.89) for meeting clinical failure criteria. The optimal cut-off score was 11 with corresponding sensitivities and specificities shown in Table 1. Lateral imaging demonstrated similar accuracy.
Conclusion(s): In contrast to previous studies, we found that the ability of pre-extubation LUS to predict reintubation in very preterm infants is only fair. This may relate to our more mature cohort or lower number of reintubations. Accuracy is increased in infants born < 28 weeks’ gestation. Future research should focus on infants at highest risk of extubation failure and consider simpler imaging protocols.