Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 2: Fetal/Neonatal Metabolic Dyscrasias
123 - Diabetes in pregnancy and early nutrition in moderate to late preterm infants: A prospective cohort study
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 123
Publication Number: 123.99
Publication Number: 123.99
.jpg)
Catherine O. Buck, MD (she/her/hers)
Assistant Professor of Pediatrics
Yale School of Medicine
Guilford, Connecticut, United States
Presenting Author(s)
Background: Diabetes (DM) in pregnancy is associated with obesity and cardiometabolic abnormalities in childhood. Our prior work has shown that preterm infants exposed to DM in pregnancy have differences in early growth trajectory compared with those not exposed to DM. The influence of early nutrition on growth patterns in preterm infants exposed to DM in pregnancy is unknown.
Objective: To examine the influence of DM exposure on daily fluid volume and calorie intake in moderate to late preterm infants.
Design/Methods: This is a secondary analysis of a cohort of moderate to late preterm (30-36 weeks) and term (>37 weeks) infants born at a single center and admitted to newborn nursery or neonatal intensive care (NICU) units 2020-2022, oversampling for exposure to DM. Bedside body composition assessments were completed through hospital discharge, and hospital nutrition information was obtained from the medical record. Maternal and infant health characteristics, nutrition information, and anthropometry assessments at birth and discharge were compared between DM groups in a bivariate analysis. Average total fluid intake per day (enteral + intravenous) was estimated using an adjusted linear mixed effects model.
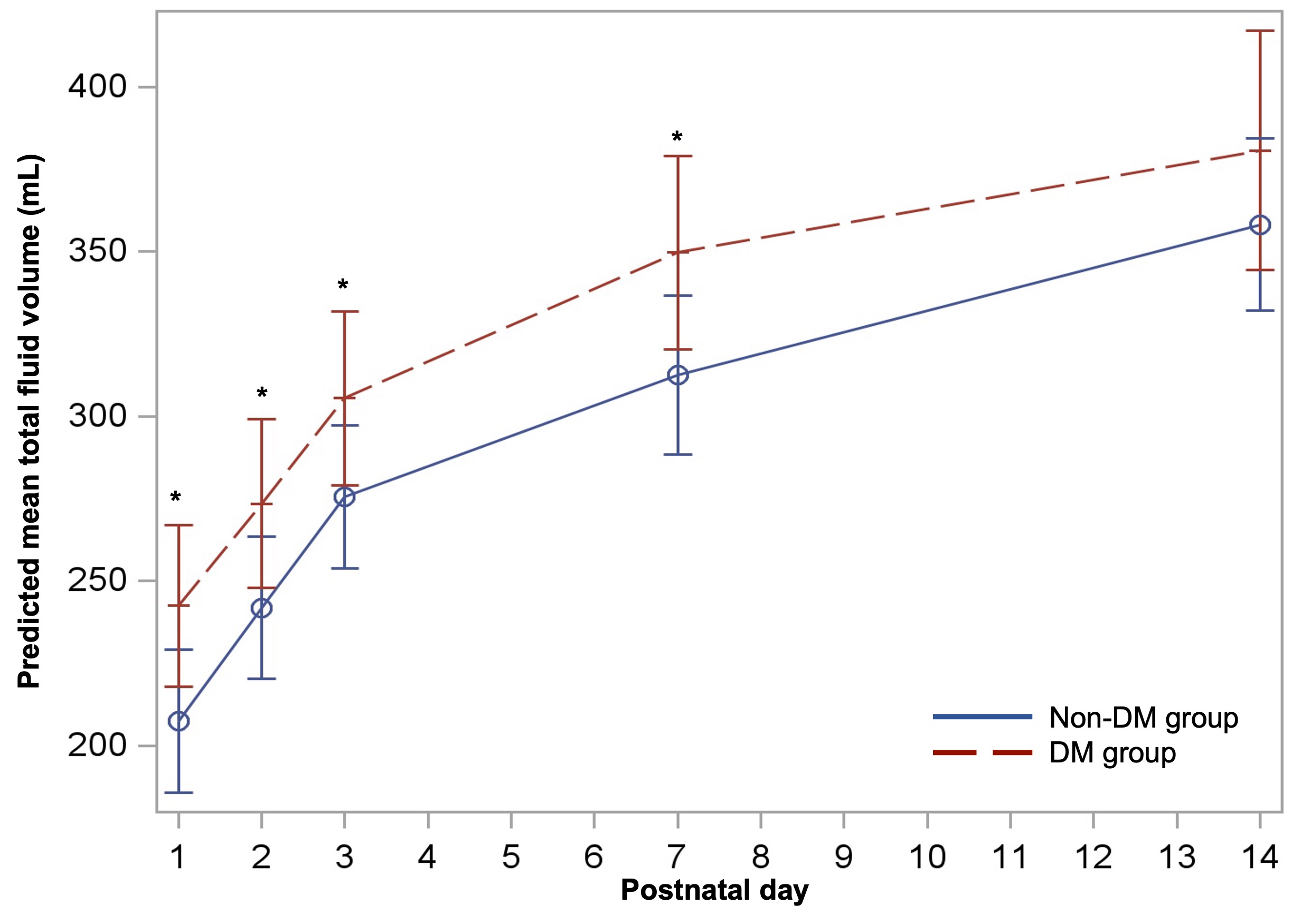
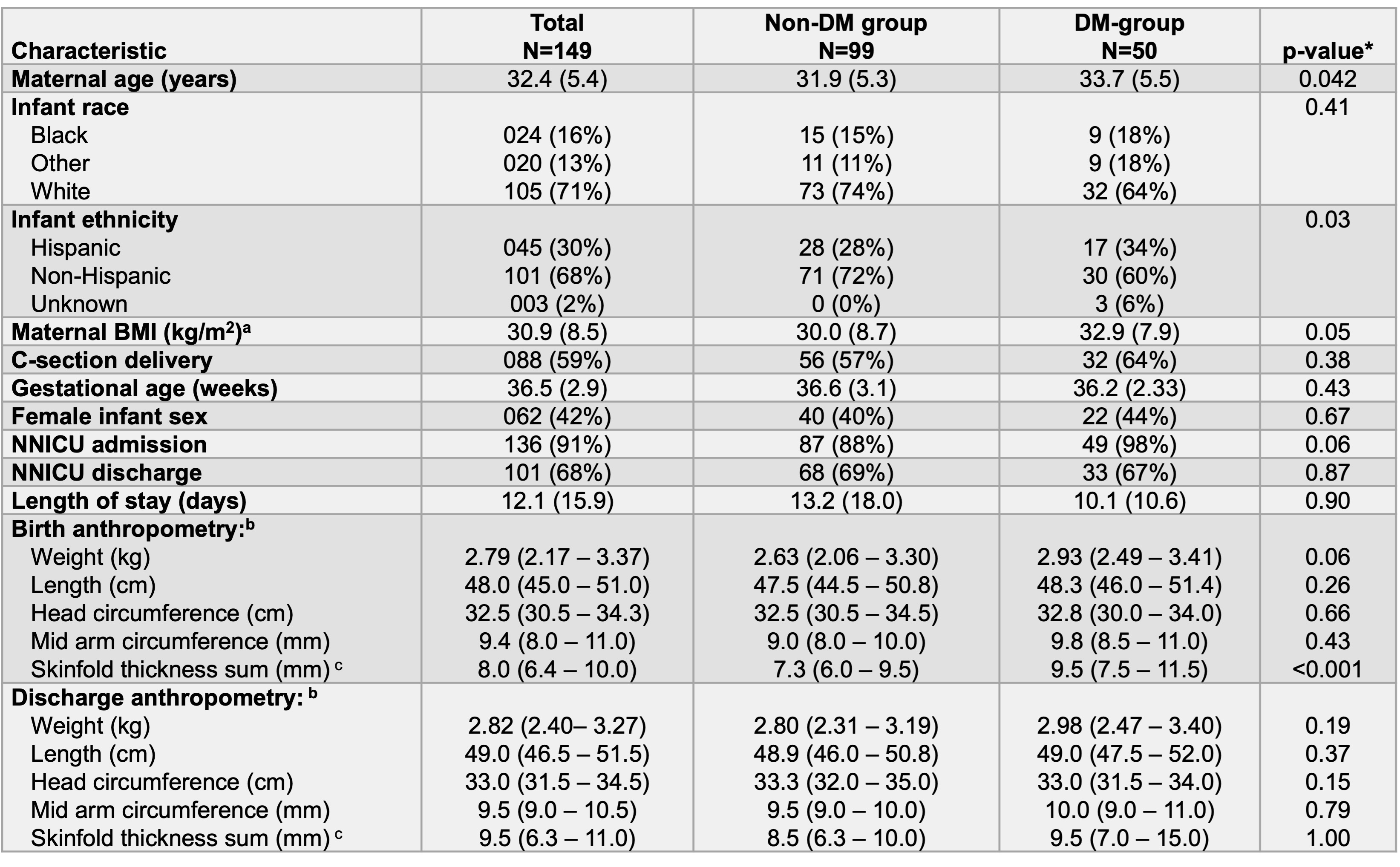
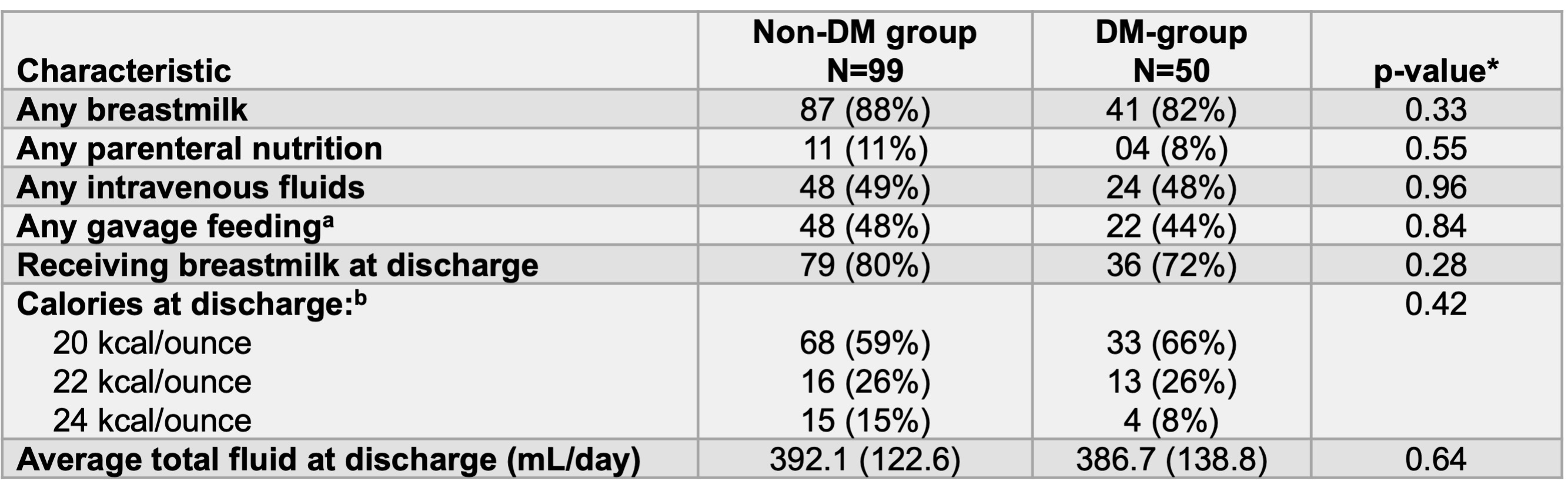
Results: Among the 149 infants included in the analysis, 33% (N=50) were exposed to DM in pregnancy. Average GA was 36.5 (±2.9) weeks, and 91% of infants were cared for in the NICU during the hospital stay (Table 1). DM-group infants had higher birth weight and skinfold thickness sum, compared with the non-DM group (Table 1). DM-group infants had higher total fluid volume in the first postnatal week, but not at hospital discharge when compared with the non-DM group (Figure 1, Table 2). The estimated mean total fluid on day 1, 2, and 7 was 207.4 (95%CI: 185.6, 229.1), 241.8 (95%CI: 220.2, 263.4), and 312.5 (95%CI: 288.4, 336.6) mL/day for the non-DM group compared with 242.4 (95%CI: 217.9, 266.9), 273.5 (95%CI:247.8, 299.1), and 349.7 (95%CI: 320.4, 380.0) mL/day for the DM group, respectively. Prescribed calories at discharge were not different between groups (Table 2), but among infants not exclusively breastfeeding, non-DM group was less likely to receive unfortified feeds at discharge (40% vs 59%, p=0.05).
Conclusion(s): In this study, exposure to DM in pregnancy was associated with higher total fluid volume per day in the first postnatal week, but not at hospital discharge. The observed differences may be related to feeding maturity in this at-risk population. The association of fluid intake with weight trajectory and adiposity outcomes requires further investigation to inform clinical practice change.