Neonatology
Session: Neonatal Neurology 4: Clinical
522 - Decreased response to anti-seizure medication in very premature infants
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 522
Publication Number: 522.1090
Publication Number: 522.1090
- VC
Veronica Caballero, MD
Fellow
Holtz Children's Hospital Jackson Memorial Hospital
Miami Springs, Florida, United States
Presenting Author(s)
Background: Neonatal seizures increase the risk of epilepsy and developmental delay. Management of neonatal seizures in premature infants is challenging because frequently the etiology cannot be confirmed and there is little evidence on which is the most effective medication to use as first line.
Objective: The objective of this study was to evaluate the response to anticonvulsant medication in premature infants when compared with full term neonates.
Design/Methods: This was a retrospective cohort study of infants with the diagnosis of neonatal seizures admitted to the Neonatal Intensive Care Unit. The study was approved by Institutional Review Board, and the need for informed consent was waived. The diagnosis of seizures was made clinically and by continuous video-electroencephalography (EEG). Seizure free state was defined by an EEG demonstrating absence of seizures for a minimum of 6 hours. Phenobarbital or levetiracetam were used as first line agents. A second medication was added if electrographic seizures persisted despite maximizing monotherapy, defined by achieving a phenobarbital level of 40 mg /dL or a levetiracetam dose of 100 mg/kg/day. Data collected included demographic and clinical characteristics related to the seizures. Mean, standard deviation and frequency were used for descriptive statistics and Chi Square analysis to assess differences between groups.
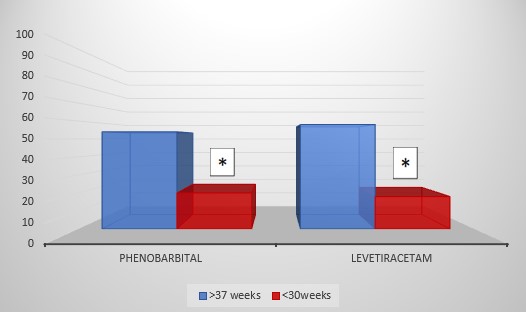
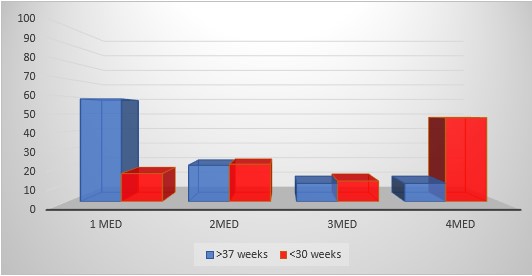
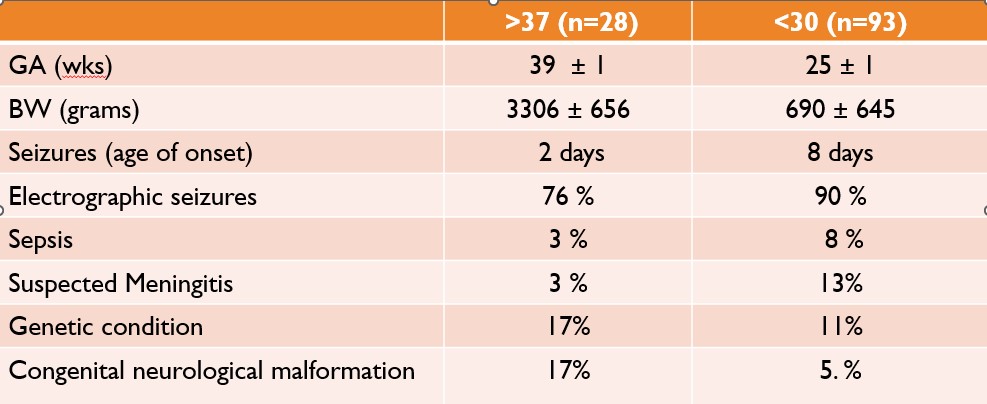
Results: Between 2019 and 2021, 123 infants met seizure criteria, 94 were < 28 weeks and 29 were > 37 weeks gestational age. Demographic and clinical characteristics of the groups, including EEG confirmation of seizures are displayed in table 1. The proportion of infants who responded to phenobarbital was significantly lower in the group of very preterm infants when compare with full term infants, 20% vs 54% (p < .024). Similarly, when levetiracetam was used as first line medication, the proportion of infants in the preterm group that responded to the treatment was significantly lower than in the full-term infants 18% vs 58% (p < 0.002) (Figure 1). While 58% of newborns > 37 weeks of gestational age responded to the first line medication, 48% of the very preterm infants needed up to 4 medications to control seizures. (Figure 2).
Conclusion(s): These results show that in a population of very preterm infants, both phenobarbital or levetiracetam are less effective than in full term infants and monotherapy failed to control seizures in this population. This suggests that seizures in the immature brain may be triggered by a different mechanism that in full term infants. It will be important to further evaluate the low therapeutic response in this population.