Neonatology
Session: Neonatal/Infant Resuscitation 1
257 - Feasibility of Volume Targeted- Positive Pressure Ventilation in Intubated Preterm Infants requiring Positive Pressure Ventilation in the Delivery Room
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 257
Publication Number: 257.3178
Publication Number: 257.3178

Ruben Vaidya, MD
Associate Professor of Pediatrics
University of Massachusetts Chan Medical School- Baystate
East Longmeadow, Massachusetts, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) has ~40% incidence in infants < 28 weeks gestation, and volutrauma, barotrauma and atelectotrauma all play key roles in its pathogenesis. Current delivery room (DR) respiratory management utilizes pressure-limited (PL) devices without any information on the delivered tidal volume (TV). Clinicians rely on chest expansion, which is known to poorly correlate with delivered TV. Our previous study demonstrated TV measurement via endotracheal tube (ETT) is feasible in DR using respiratory function monitor (RFM); and there is high degree of intra and interpatient variability in TV, potentially leading to volutrauma and atelectotrauma.
Objective: For this study our objectives were: 1. Assess feasibility of providing Volume targeted- Positive Pressure Ventilation (VT-PPV) in intubated preterm in the DR; and 2. To compare the delivered TV range with VT-PPV, to a historic study cohort, where infants received routine PPV via ETT.
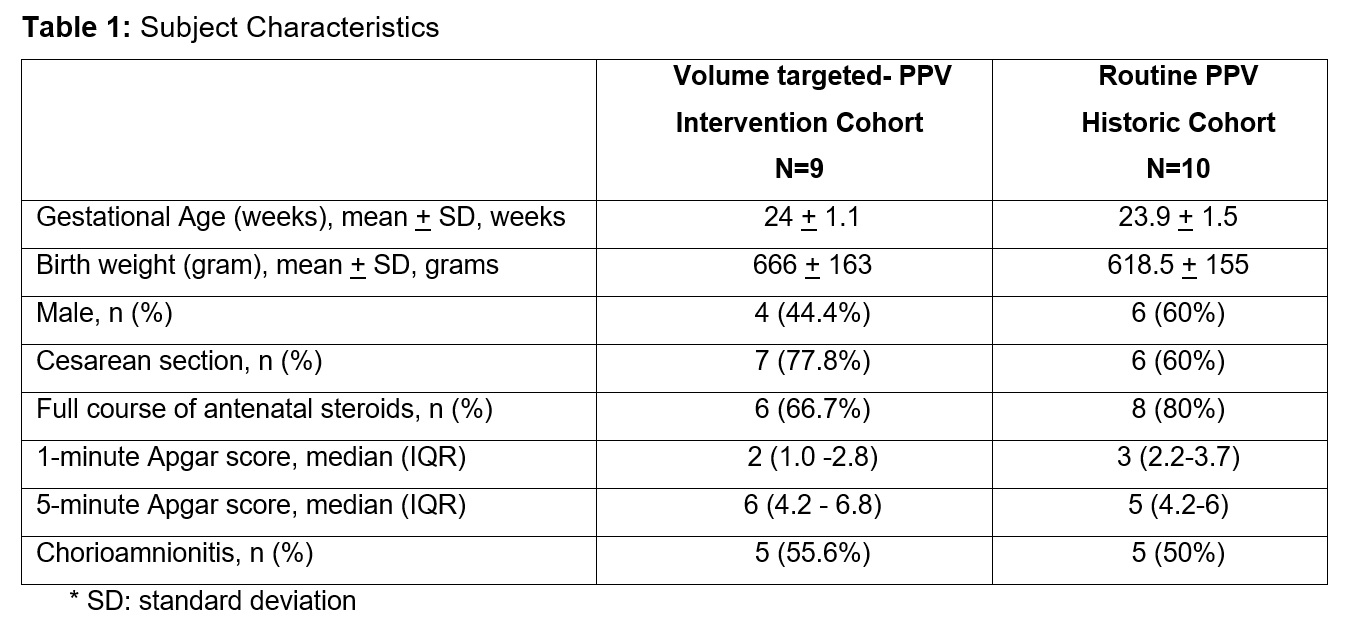
Design/Methods: Infants < 32 weeks GA requiring PPV through the ETT in DR were enrolled. In the intervention cohort (VT-PPV), providers had access to TV measurement from RFM in real time and were able to alter peak inspiratory pressures (PiP) to target TV at 4-6 ml/kg range. Being a feasibility study, after a convenience sample of 10 patients was obtained, the study was closed. Data from 1 patient was lost due to loss of battery power on the RFM. Data was compared with historic study cohort (HC), where providers were blinded from RFM measurements and they provided routine PPV via ETT per standard. A T-piece resuscitator is used for PPV in our institute. This study was approved by Baystate Health IRB.
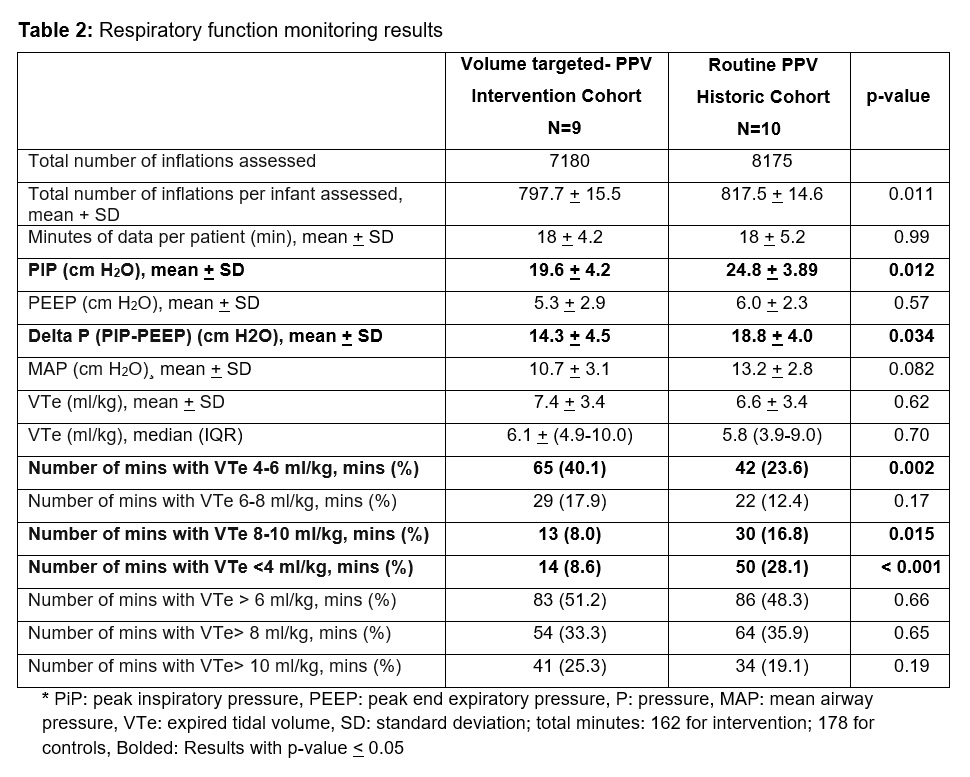
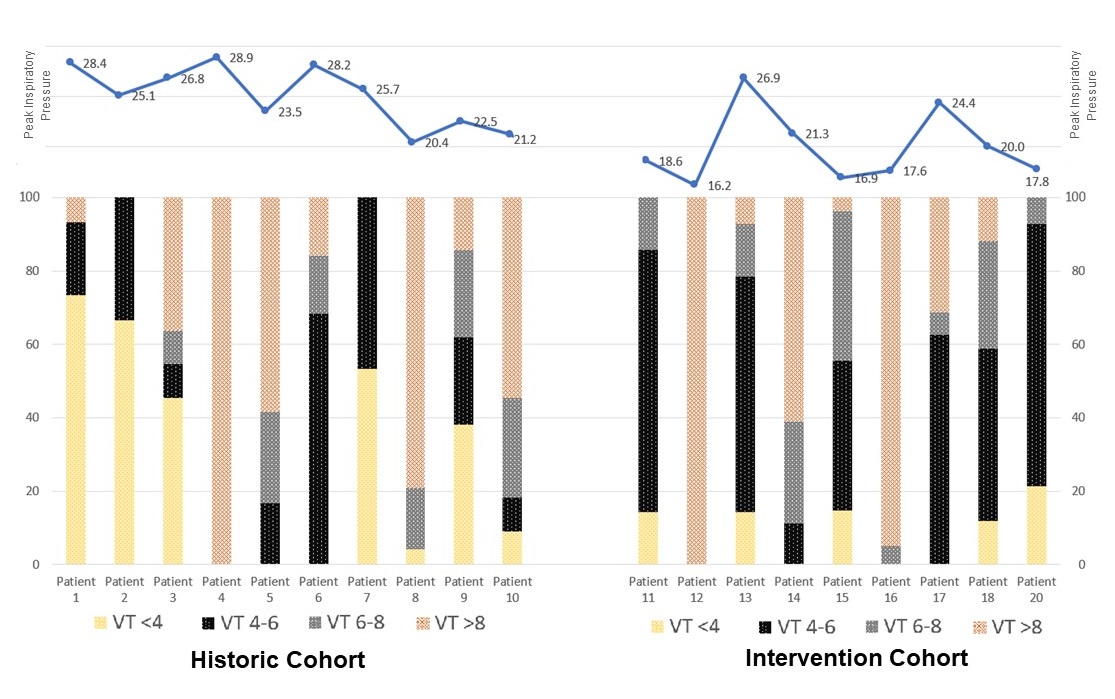
Results: Basic demographic information of the subjects are reported in Table 1. Nine patients were provided VT-PPV in DR (total 162 mins, mean 18 mins/patient, 7180 individual breaths), and this was compared with 10 historic study cohort patients (total 178 mins, mean 17.8 mins/patient, 8175 individual breaths). The TVs were averaged over 1 min interval automatically by the RFM. Goal TV of 4-6 ml/kg was provided 40.1% of times (vs 23.6% in HC, p=0.002), low TV ( < 4ml/kg) was provided 8.6% of times (vs 28.1% in HC, p= < 0.001) and high TV (>6ml/kg) was provided 51.2% of times (vs 48.3% in HC, p=0.66). TV >8ml/kg and >10ml/kg were similar in the 2 cohorts.
Conclusion(s): Providing volume targeted positive pressure ventilation in intubated preterm infants may be feasible in DR. VT-PPV resulted in increased number of breaths in target range. Further studies are needed to evaluate the potential benefits of VT-PPV in the DR.