Developmental and Behavioral Pediatrics
Session: Developmental and Behavioral Pediatrics 5: ADHD and Learning
607 - Association of ADHD Diagnosis with Blood Pressure Severity, Target Organ Injury, and Cardiovascular Health at Baseline in Youth with Hypertension Disorders
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 607
Publication Number: 607.1834
Publication Number: 607.1834
- AP
Ashna Pudupakkam, MD (she/her/hers)
Pediatric nephrology fellow
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Attention deficit hyperactivity disorder (ADHD) is frequently managed with stimulant medications in the pediatric population. While many stimulant medications are associated with an increased risk of hypertension, whether ADHD is associated with worse blood pressure severity or cardiovascular health in youth with diagnosed hypertension disorders is unclear.
Objective: To determine the association of ADHD diagnosis with blood pressure severity, target organ injury, and cardiovascular health in youth referred for hypertension disorders.
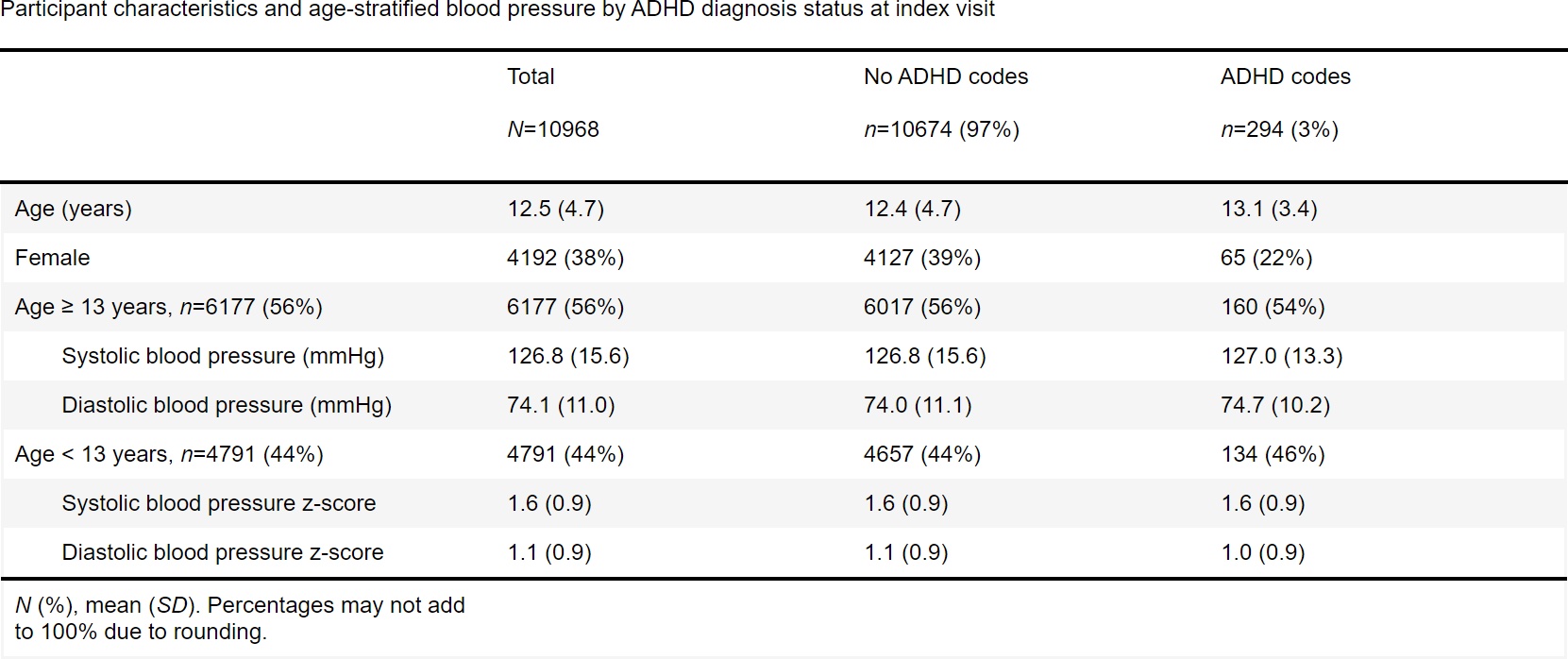
Design/Methods: Cross-sectional analysis of baseline data from the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO), a multisite Registry that retrospectively collects electronic health record data validated by manual record review. We included patients with ICD-10 codes for hypertension disorders at the index visit at subspecialty hypertension clinics who were aged < 19 years. We excluded patients with ICD-10 code-identified pregnancy, kidney failure on dialysis, or kidney transplantation. Our exposures were an ICD-10 code visit diagnosis for ADHD at the index visit. Our outcomes were blood pressure severity at the index visit, obesity by BMI or weight-for-length percentiles, and target organ injury, dyslipidemia, and hyperglycemia by ICD-10 visit diagnoses. We used unadjusted generalized linear models.
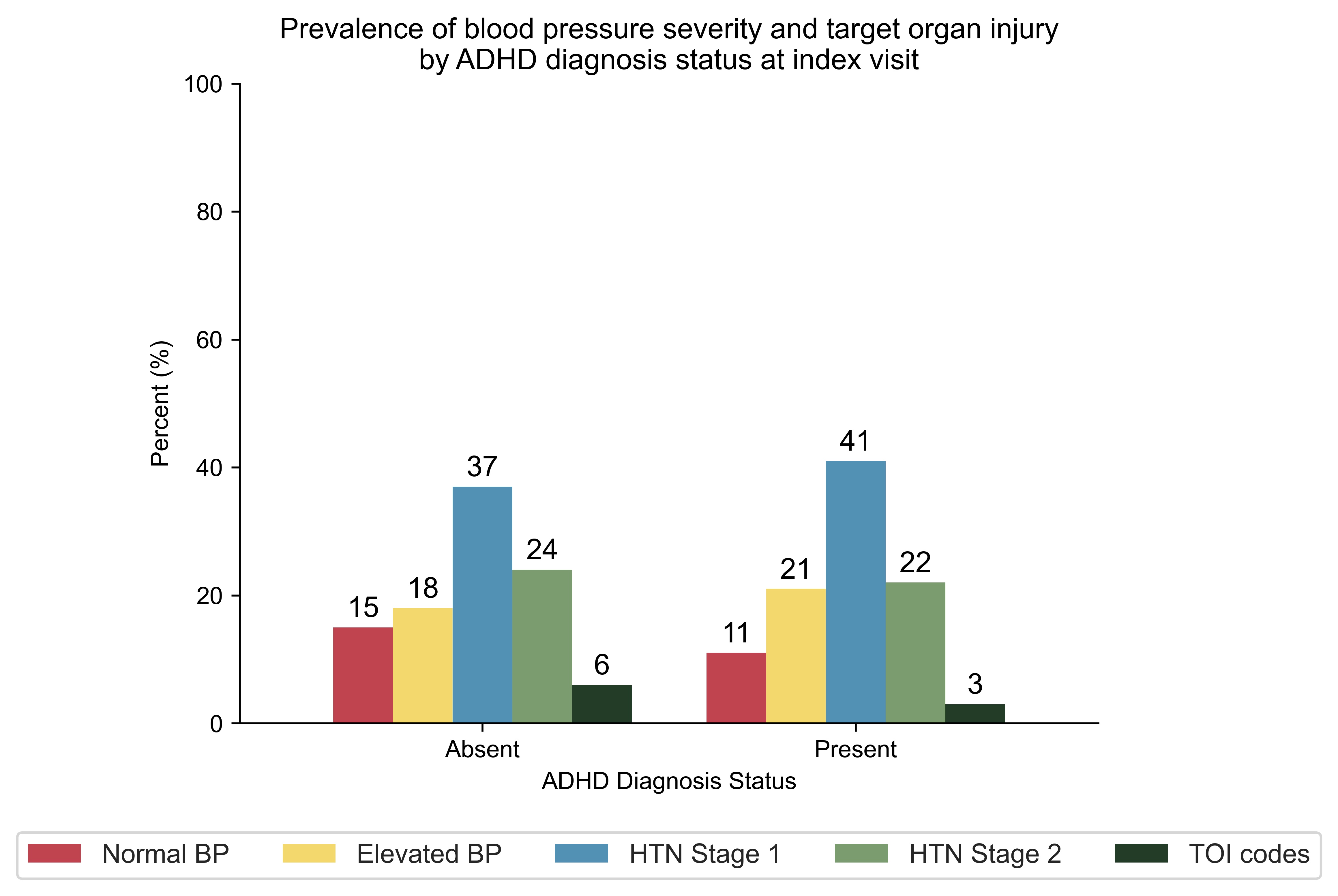
Results: In our cohort, 3% of participants (294 out of 10,968) had a diagnosis code of attention deficit hyperactivity disorder. Participants with a diagnosis code of ADHD did not have worse hypertension or worse cardiovascular health, except for a 51% lower risk of target organ injury and a 46% lower risk of hyperglycemia.
Conclusion(s): We found that youth with attention deficit hyperactivity disorder referred for hypertension did not have worse hypertension, cardiovascular health, or target organ injury. This study may have been impacted by variation in pharmacologic management of ADHD, variability in coding or underdiagnosis of ADHD, and variation in referral patterns. The lower risk of target organ injury may be due to an earlier referral pattern for patients with ADHD. Potential limitations include a lack of longitudinal blood pressure data and ambulatory blood pressures as this study was based on blood pressure data collected from the index visit only. In future studies, we plan to further develop and validate case definitions of our exposures and outcomes. We also plan to collect ambulatory blood pressure monitoring data in youth referred for hypertension to determine if there is an association between ADHD and white coat hypertension.
.jpg)