Neonatology
Session: Neonatal Neurology 2: Clinical
19 - Timing of Initiation of Therapeutic Hypothermia and Association with Short-Term Outcomes in Neonates with Hypoxic-Ischemic Encephalopathy
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 19
Publication Number: 19.216
Publication Number: 19.216
.jpg)
Christine Pazandak, MD, MSCI, MPH (she/her/hers)
Assistant Professor
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Whole body therapeutic hypothermia (TH) is the standard of care for treating infants diagnosed with moderate to severe hypoxic-ischemic encephalopathy (HIE) and has been shown to be most beneficial for those diagnosed with moderate HIE. Although there is evidence in pre-clinical animal models and small retrospective patient cohorts that support the idea that earlier cooling provides better neuroprotection, this hypothesis has not been investigated in clinical trials due to ethical concerns. Post-hoc analysis of the large, randomized controlled trials establishing the efficacy of TH have not yielded sufficient differences in time to initiate of TH due to the process of consent and randomization.
Objective: To determine the association between time to initiate TH after birth and short-term outcomes in infants with moderate and severe HIE.
Design/Methods: This retrospective cohort study included neonates born at Parkland Hospital from 2009-2023 with moderate or severe HIE and treated with TH within 6 HOL. Short-term outcomes in those initiating TH at < 4 HOL were compared to infants who initiated TH at > 4 hours. Logistic regression modeling was used to determine adjusted odds ratios (aOR) of short term outcomes based on time of initiation of TH.
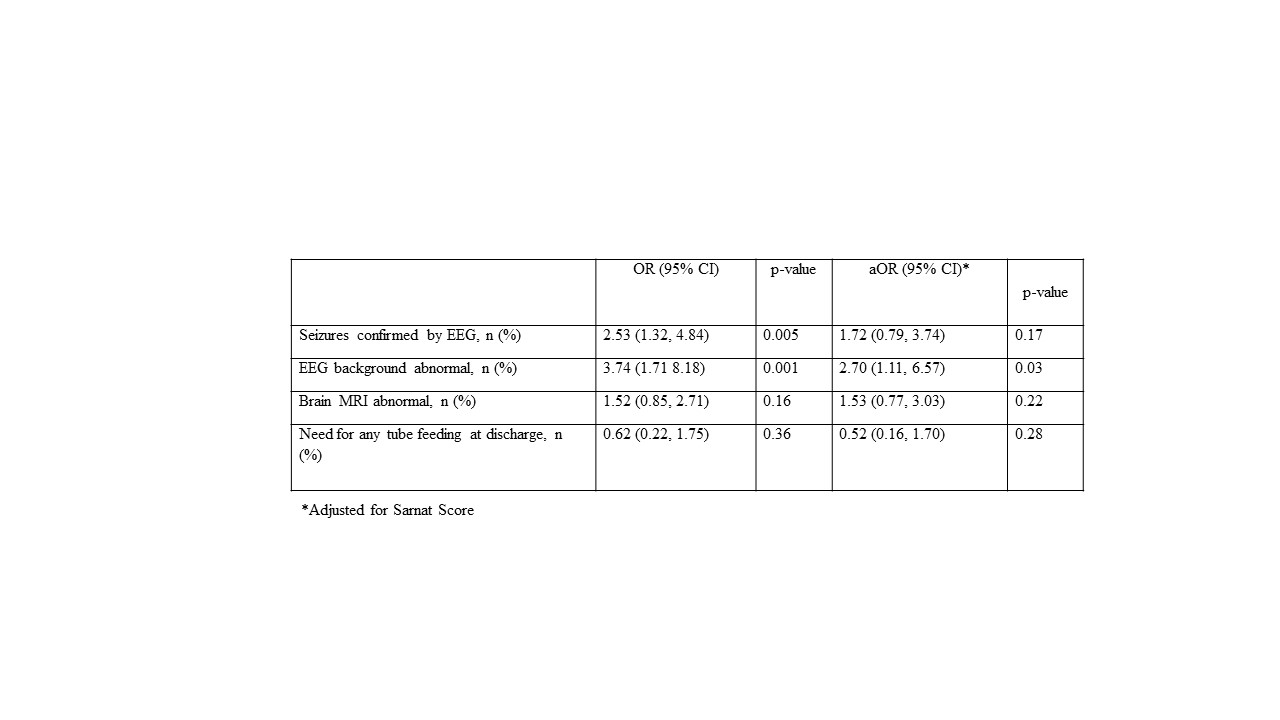
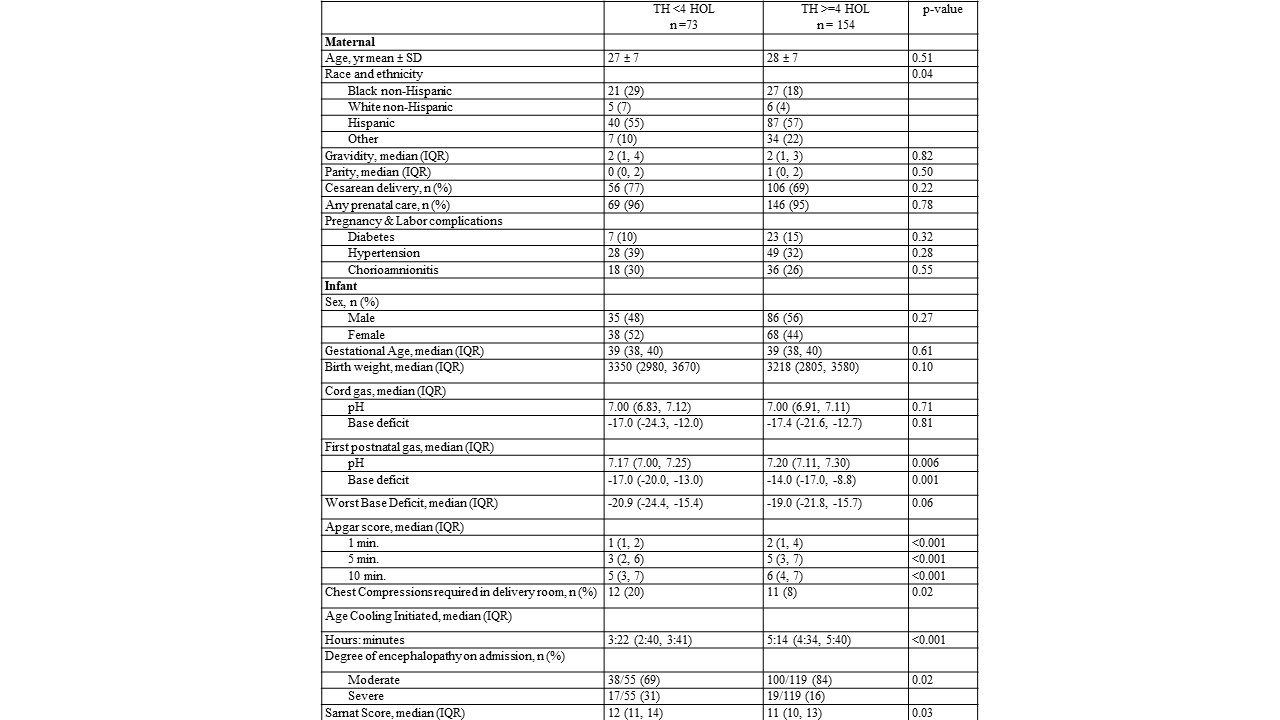
Results: A total of 227 patients were diagnosed with HIE during the study period. Those initiating TH at < 4 HOL (n=73) differed significantly from those who initiated TH at >4 HOL (n=154); specifically, they were more likely to have severe HIE (31% vs. 16%; p=0.02), higher Sarnat score [12 (11, 14) vs. 11 (10, 13); p=0.03] and lower Apgar scores at 5 and 10 MOL [3 (2, 6) vs. 5 (3, 7); p< 0.001 and 5 (3, 7) vs. 6 (4, 7); p< 0.001, respectively]. In logistic regression models adjusting for Sarnat score, there was an increased aOR of abnormal background EEG in those initiating TH earlier [2.70 (1.11, 6.57); p=0.03], but no differences in other short term outcomes including seizures [1.72 (0.79, 3.74); p=0.17], abnormal brain MRI [1.53 (0.77, 3.03); p=0.22], or need for any gastric tube feeding at discharge [0.52 (0.16, 1.70); p=0.28]. In exploratory analyses of the moderate HIE subgroup, no differences were detected in short term outcomes based on timing of initiation of TH.
Conclusion(s): Neonates with severe HIE are more likely to initiate TH earlier than those with moderate HIE. Correlation of short-term outcomes with time to initiate TH is highly confounded by those with severe HIE who are readily diagnosed. There is a need to focus efforts on improving the initiation of TH for those diagnosed moderate HIE in order to study effects on short-term outcomes.
.jpg)