Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 2
489 - Pediatric Critical Care Medicine Education in the Pediatric Residency of Honduras: A Needs Assessment
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 489
Publication Number: 489.79
Publication Number: 489.79

Pablo J. Napky Raudales, MD, FAAP (he/him/his)
Pediatric Critical Care Medicine Fellow
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Children in Honduras die at a much higher rate than in the US. Due to lack of human and physical resources, most critically ill children receive care outside of intensive care units by general pediatricians. Thus, essential knowledge and skills upon graduating residency may differ from other countries.
Objective: To better understand the educational needs of pediatric residents in Honduras in the care of critically ill children.
Design/Methods: Using survey methodology, we performed a cross-sectional study of the 2 pediatric residencies in Honduras. An electronic survey was developed with local educator input. Items focused on perceptions of essential critical care competencies for graduating residents, current educational approach, gaps, and effective learning strategies. Current residents and faculty were invited to participate via email in Oct 2023.
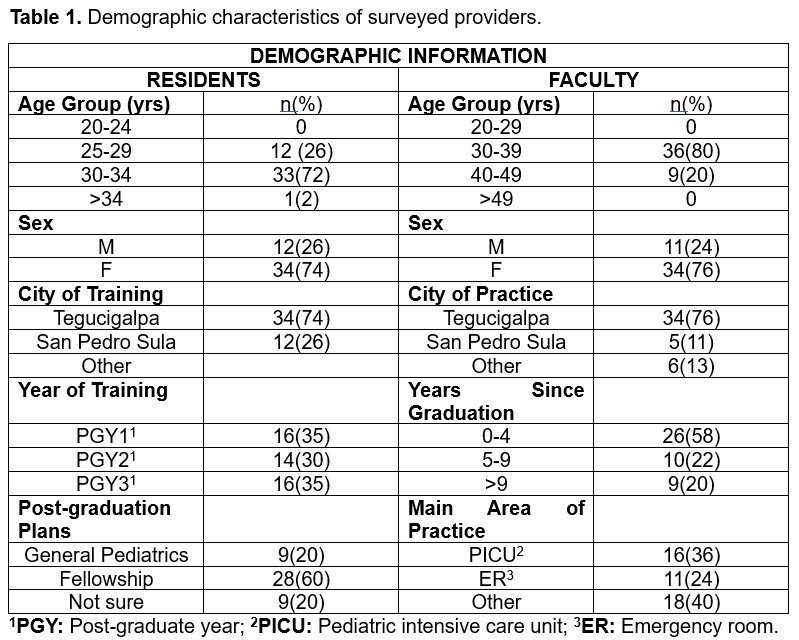
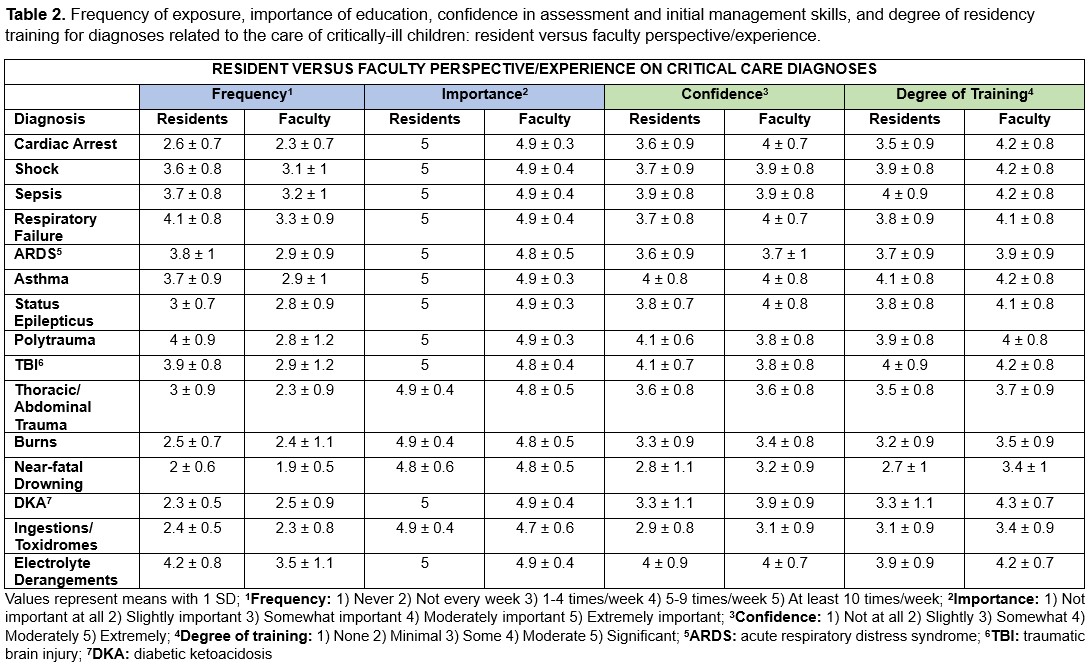
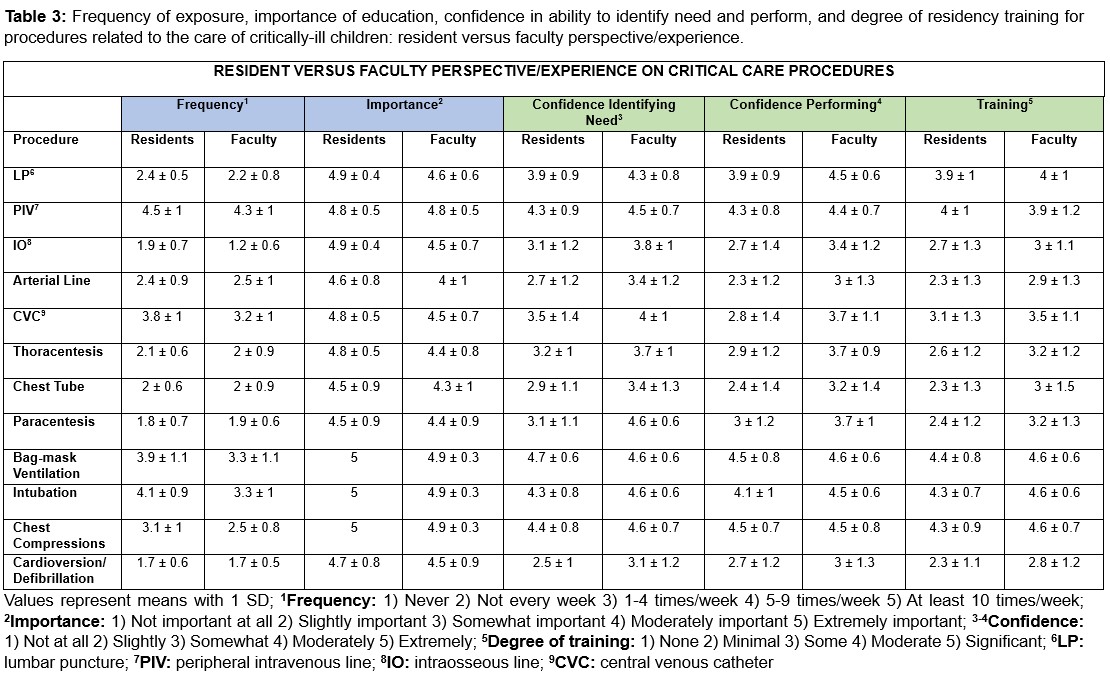
Results: 49/96 (51%) residents and 45/91 (49%) faculty responded to the survey, with similar numbers of residents from each training year. (Table 1) Most faculty were within 10 yrs of graduation. Most residents (91%) and faculty (82%) believe critical care education to be extremely important. Half of residents (52%) were only slightly or somewhat comfortable assessing critically ill children, whereas 33% of faculty reported similar comfort upon graduation. Most faculty and residents agreed the pre-identified diagnoses were important in residency education, but treatment frequency, confidence and degree of training in residency varied. (Table 2) Severe dengue, critical care transport, oncologic complications, and point-of-care ultrasound were additional topics of importance. Multiple procedures relevant to resuscitation (eg, intraosseous line, cardioversion/defibrillation) were identified as highly important, yet both groups reported lower confidence and degree of residency training. (Table 3). Residents receive critical care education mostly through lectures, self-directed learning, and bedside teaching. About two-thirds of each group reported being moderately to extremely satisfied with the current education, with 57% residents and 50% faculty needing to supplement their education. Residents and faculty identified problem-based learning, direct patient care, and bedside teaching as most effective, and have interest in simulation-based education.
Conclusion(s): We identified essential competencies in the care of critically ill children for graduating pediatricians in Honduras and areas for additional educational growth, which can inform the development of learning resources to advance the care of this vulnerable population.