Obesity
Session: Obesity 2
610 - Relationships Between Night-Eating, Obesity, Daytime Sleepiness and Chronotype in Children Presenting for Sleep Evaluation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 610
Publication Number: 610.3298
Publication Number: 610.3298

Abigail R. Strang, MD (she/her/hers)
Pediatric Pulmonologist
Sidney Kimmel Medical College at Thomas Jefferson University
Garnet Valley, Pennsylvania, United States
Presenting Author(s)
Background: Circadian rhythms are present in all organisms with multisystem impact. Literature in adults suggests that eating later in the day and insufficient sleep leads to circadian misalignment, associated with obesity and daytime sleepiness. There is limited pediatric research on these relationships. As the prevalence of pediatric obesity increases, it is especially important to understand these relationships to provide optimal anticipatory guidance on diet and sleep.
Objective: The objective of this study is to describe chronotype, eating timing, and daytime sleepiness in a cohort of children presenting for sleep medicine evaluation and to evaluate relationships between eating time, chronotype, daytime sleepiness, and obesity.
Design/Methods: This is an IRB-approved cross-sectional, survey-based study completed May-August 2023. Eligibility criteria included age 11-17 years, English-speaking, and developmentally able to understand surveys. Recruitment, consent/assent and survey administration were completed during sleep medicine clinic visit. 3 validated surveys were administered: The Epworth Sleepiness Scale for Children and Adolescents (ESS-CHAD, higher scores=more sleepiness), The Morningness Eveningness Questionnaire (MEQ, used for identifying chronotype), and the Night Eating Diagnostic Questionnaire (NEDQ, categories of night eating based on scoring criteria). Electronic medical records were reviewed for BMI and BMI Z-score. Descriptive and comparative statistics were performed to compare night-eaters and non night-eaters.
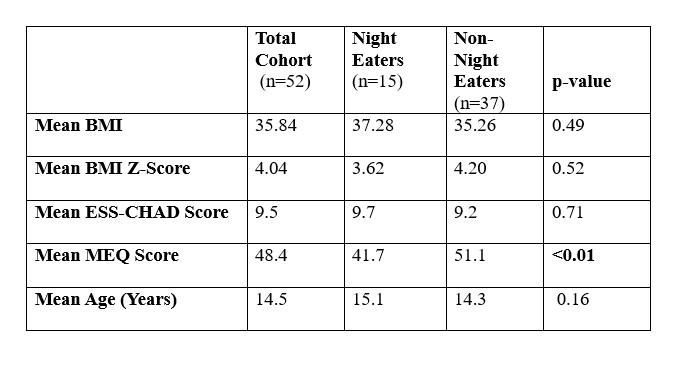
Results: Study participants (n=52) were 58% male, mean age 14.5 years (SD= 1.93). The mean BMI was 35.8 kg/m2 (SD= 11.5), mean BMI Z-score was 4.0 (SD= 3.6), 75% were obese, 53% had increased daytime sleepiness, and 29% were night-eaters. Among the night eating group (n=15), mean BMI was 37.3 (SD=7.6), BMI Z-score of 3.6 (SD=2.4), 87% were obese, 53% were abnormally sleepy, and 47% had a moderate evening chronotype. Among the non-night eating group (n=37) mean BMI was 35.3 (SD=12.8), mean BMI Z-score was 4.2 (SD= 4), 70% were obese, 54% were abnormally sleepy, and 76% had an intermediate chronotype. See Table I for comparisons between groups.
Conclusion(s): Night-eating is associated with evening chronotype in this pediatric population presenting for sleep-medicine evaluation. There were no observed differences in rates of daytime sleepiness or obesity between night-eaters and non night-eaters. BMI was overall very high in the entire cohort, which affected analysis. Further studies to evaluate these relationships in a larger population with a more varied BMI are necessary.