Asthma
Session: Asthma 2
196 - The effects of SARS-CoV-2 infection on incident asthma in children: a sub-analysis of known asthma risk factors
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 196
Publication Number: 196.36
Publication Number: 196.36

James P. Senter, MD, MPH (he/him/his)
Hospitalist Physician
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Respiratory viral infections, particularly rhinovirus and RSV, are risk factors for recurrent wheezing and/or asthma in infants and small children. Less is known about the impact of coronaviruses on the development of asthma.
Objective: We sought to determine the association between SARS-CoV-2 infection and the risk of asthma diagnosis in children and how it may relate to other well-described asthma risk factors.
Design/Methods: This is a retrospective longitudinal cohort study of children from birth to age 16 within the Children’s Hospital of Philadelphia Care Network who received PCR testing for SARS-CoV-2 (primary exposure) between March 1, 2020 and February 28, 2021. Subjects had at least one well child visit in the year preceding PCR test and were followed for 18 months following PCR test. The primary outcome of new asthma diagnosis was defined using ICD codes and medication prescriptions. Multivariable Cox regression models assessed the hazard ratio of incident asthma diagnosis between SARS-CoV-2 PCR positive and negative groups. Regression models accounted for demographic characteristics, socioeconomic variables, and atopic comorbidities.
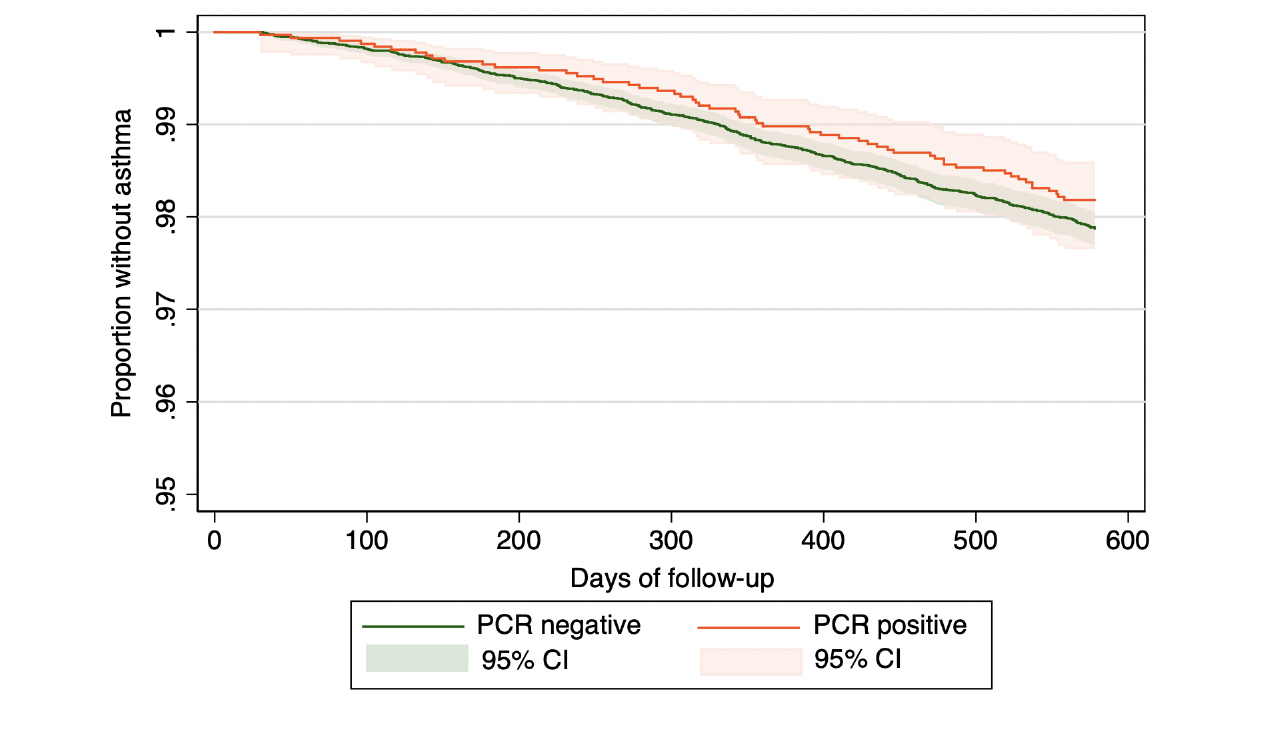
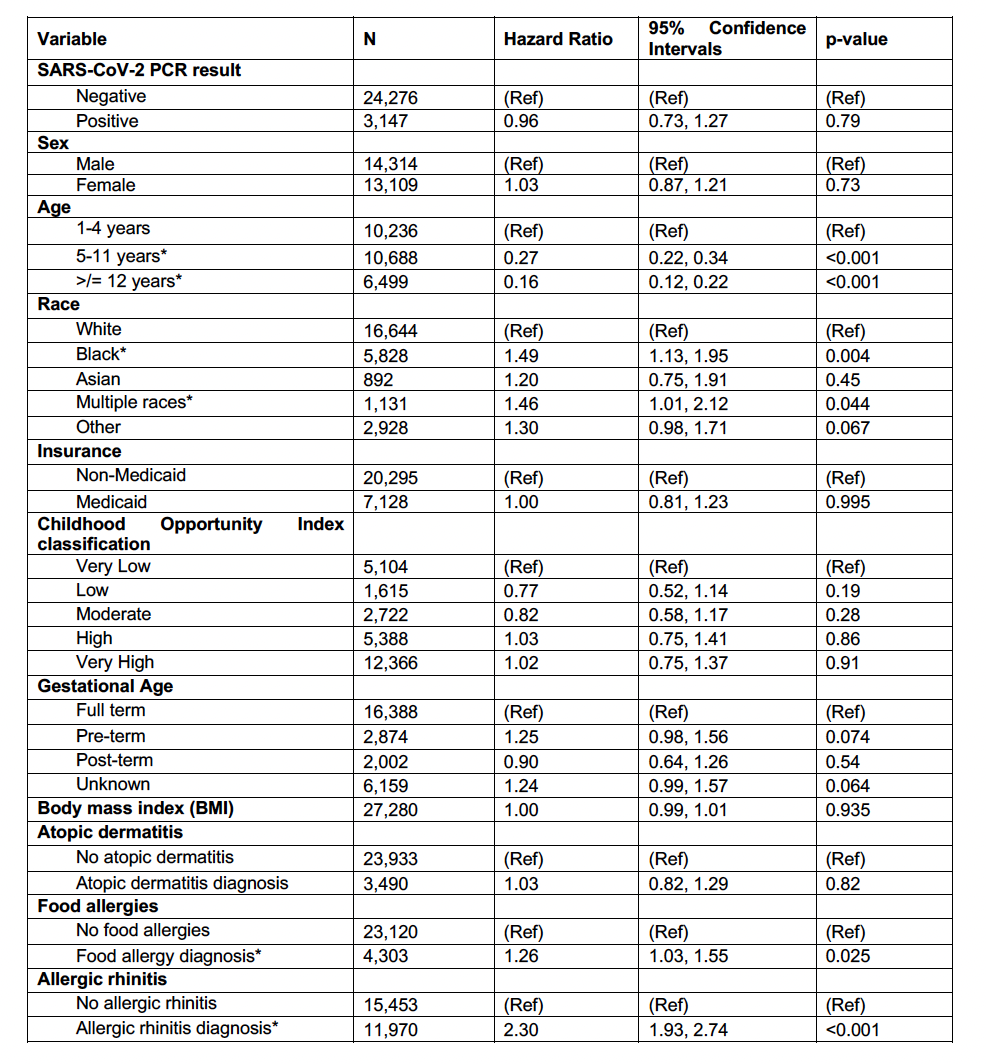
Results: There were 27,423 subjects included in the study. Among SARS-CoV-2 positive subjects, 1.81% (n=57) were diagnosed with asthma in the subsequent 18 months compared to 2.13% (n=516) of SARS-CoV-2 negative subjects. In adjusted analyses, SARS-CoV-2 PCR positivity had no significant effect on the hazard of new asthma diagnosis when controlling for effects of demographic, socioeconomic, and atopic risk factors (HR: 0.96; p = 0.79). Across the study cohort, Black race (HR: 1.49; p = 0.004) and diagnoses of food allergies (HR: 1.26; p = 0.025) and allergic rhinitis (HR: 2.30; p < 0.001) significantly increased the hazard of new asthma diagnosis. In subgroup analyses by age, pre-term birth (HR: 1.48; p = 0.005) and body mass index (HR: 1.13; p < 0.001) also significantly increased the hazard of new asthma diagnosis for children < 5 years old.
Conclusion(s): During the time period where it was the predominant modality of SARS-CoV-2 testing, SARS-CoV-2 PCR positivity was not associated with new asthma diagnosis, while Black race and atopic comorbidities were positively associated. This study refines our knowledge of the long-term respiratory effects of SARS-CoV-2 infection in children and adds to our growing understanding of how SARS-CoV-2 may influence asthma development in pediatric patients.