Neonatology
Session: Neonatal/Infant Resuscitation 3
288 - Evaluating the Impact of Briefing on Complex Neonatal Resuscitation Performance and Workload
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 288
Publication Number: 288.3033
Publication Number: 288.3033

Rebecca Miller, MD, MSc (she/her/hers)
Neonatal Fellow
NewYork-Presbyterian Komansky Children’s Hospital
Manhattan, New York, United States
Presenting Author(s)
Background: The Neonatal Resuscitation Program (NRP) recommends briefing prior to deliveries. While role delegation & equipment checks are standard elements, “discussion of the clinical context” may be variable. Limited studies describe the impact of pre-delivery briefing, & its different components on performance & workload.
Objective: To assess the impact of expanded briefing (ExpB) on time to performance of critical skills, performance of the NRP algorithm & individual workload compared to limited briefing (LimB)/no briefing (NoB) prior to simulated scenarios of neonatal resuscitation.
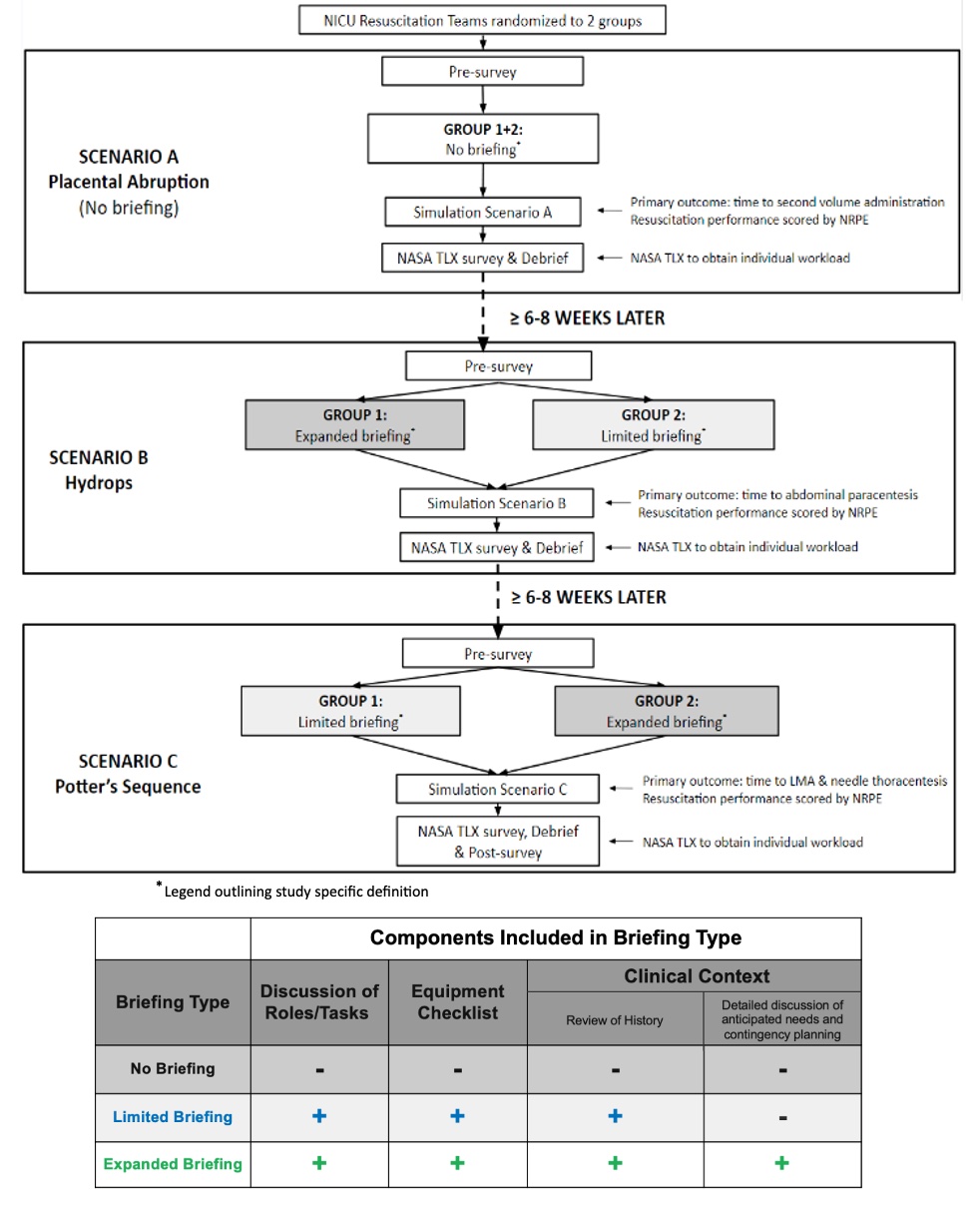
Design/Methods: 10 teams were recruited to participate in 3 delivery room scenarios utilizing a SimNewB manikin (Laerdal Medical) (Figure 1). In scenario A, no history was provided. In scenarios B & C, performance of a “critical skill” could be anticipated from the history [B: paracentesis; C: laryngeal mask airway (LMA) & needle thoracentesis]. In scenario A, no teams briefed. In scenario B, both groups performed a scripted briefing (Group 1:ExpB & Group 2:LimB). In scenario C, groups crossed over. Time to performance of scenario specific critical skill(s) & overall performance were recorded. The NASA Task Load Index (NASA TLX) was used to assess workload. Wilcoxon rank-sum was utilized.
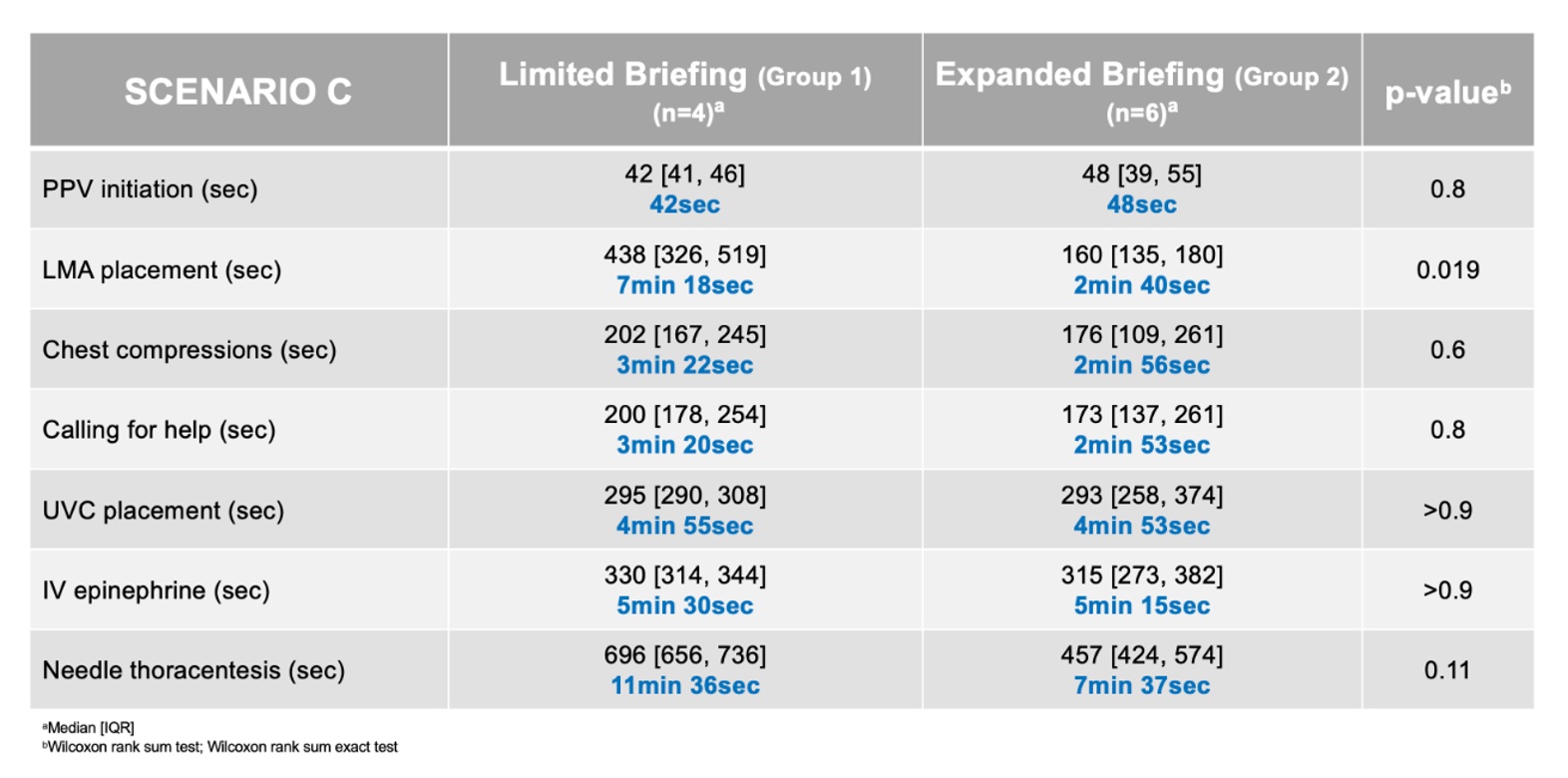
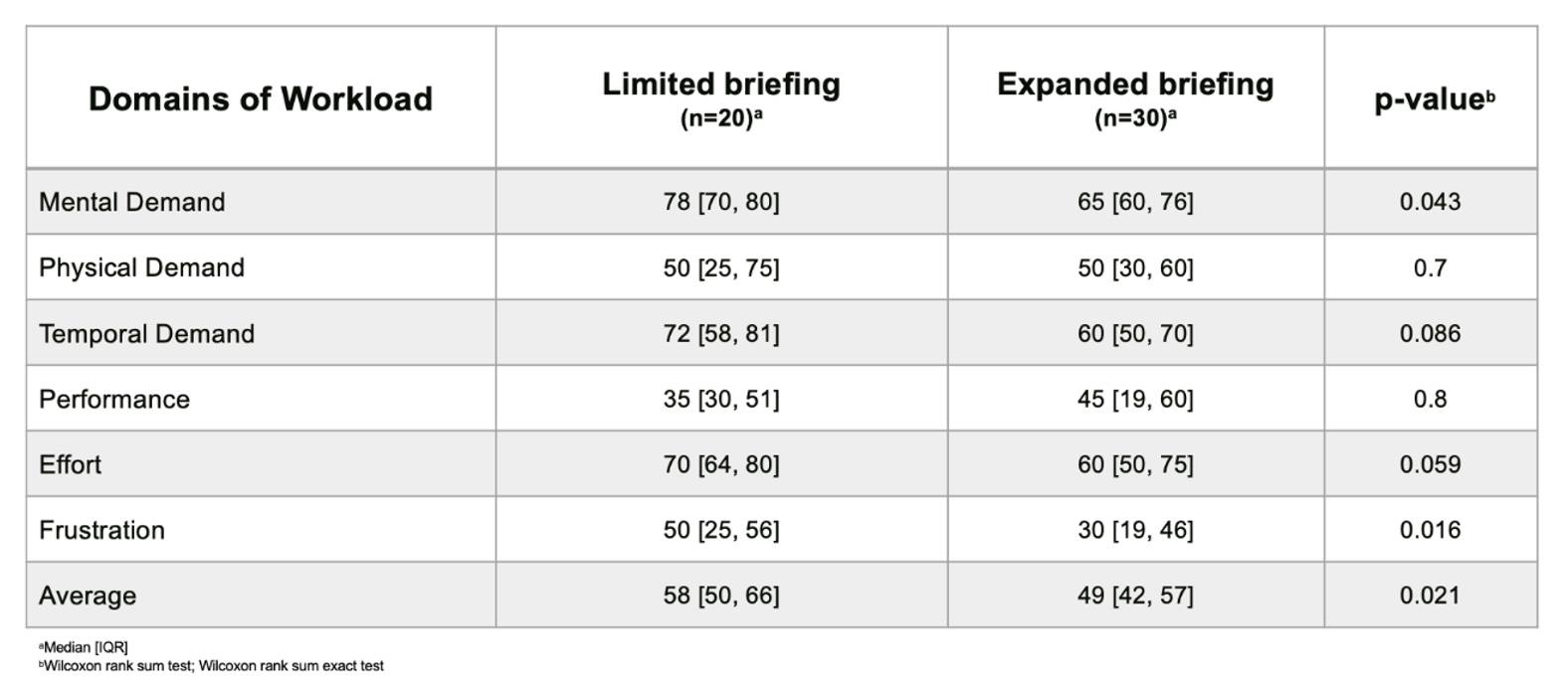
Results: 55 participants of similar experience were recruited. In scenario A (NoB) there were no differences in performance between groups. In scenario B, the ExpB group performed paracentesis faster than the LimB group (8min 34sec vs 11min 30sec; p=0.3). In scenario C, the ExpB group placed an LMA faster than the LimB group (2min 40sec vs 7min 18sec; p=0.019). Needle thoracentesis was performed faster in the ExpB vs LimB group (7min 37sec vs 11min 36sec; p=0.11) (Table 1). There was a reduction in workload when any briefing was performed (scenario B vs A) (NASA TLX score 48/100 vs 62/100; p=0.002). Moreover, ExpB reduced workload compared to LimB in scenario C (NASA TLX score 49/100 vs 58/100; p=0.021), with a notable reduction in frustration (30/100 vs 50/100; p=0.016) (Table 2).
Conclusion(s): Any pre-delivery briefing expedites performance of the algorithm & critical interventions in simulated neonatal resuscitations. Performing an ExpB reduced average workload, with a noteworthy reduction in frustration, which may impact resuscitation performance. Development of a standardized template for facilitating discussion of the clinical context for any resuscitation is essential, particularly in cases where additional/rarely performed interventions may be required.