Neonatology
Session: Neonatal General 1: NICU Care
49 - Mental Health Support and Screening for Mood Disorders for Caregivers in the NICU: Is the Call to Arms Being Answered?
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 49
Publication Number: 49.433
Publication Number: 49.433
- ML
Megan Lagoski, MD (she/her/hers)
Attending Physician, Assistant Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Perinatal mood and anxiety disorders (PMADs) affect 15-20% of women during the peripartum period. PMADs are a significant risk factor for maternal suicide. The AAP recommends routine postpartum depression screening at all well child visits. Mothers of infants in the Neonatal Intensive Care Unit (NICU) have a 25-30% higher prevalence of PMADs compared with the general population but are not regularly followed, leading to a gap in mental health care. The majority of PMADs are undiagnosed, and, if recognized, are often untreated which can interfere with healthy infant development and parent-child bonding.
Objective: 1. Describe the current state of screening for PMADs in level IV NICUs across the Children’s Hospitals Neonatal Consortium (CHNC)
2. Determine if a link exists between standardized formal screening and the presence of additional mental health professionals (MHPs)
Design/Methods: We surveyed the 44 NICUs participating in the CHNC. Responders were designated as local experts. Multiple responses per center were reviewed and variations in answers were reconciled by direct communication. Questions were asked regarding presence of NICU specific MHPs and screening practices for PMADs. Types of mental health screening performed was grouped into formal screens with validated tools, a combination of formal and informal, and informal-only screens. A standardized ratio of 1:20 MHPs per patients was used to adjust for variations in unit size. Kruskal-Wallis test was applied to examine the relationships.
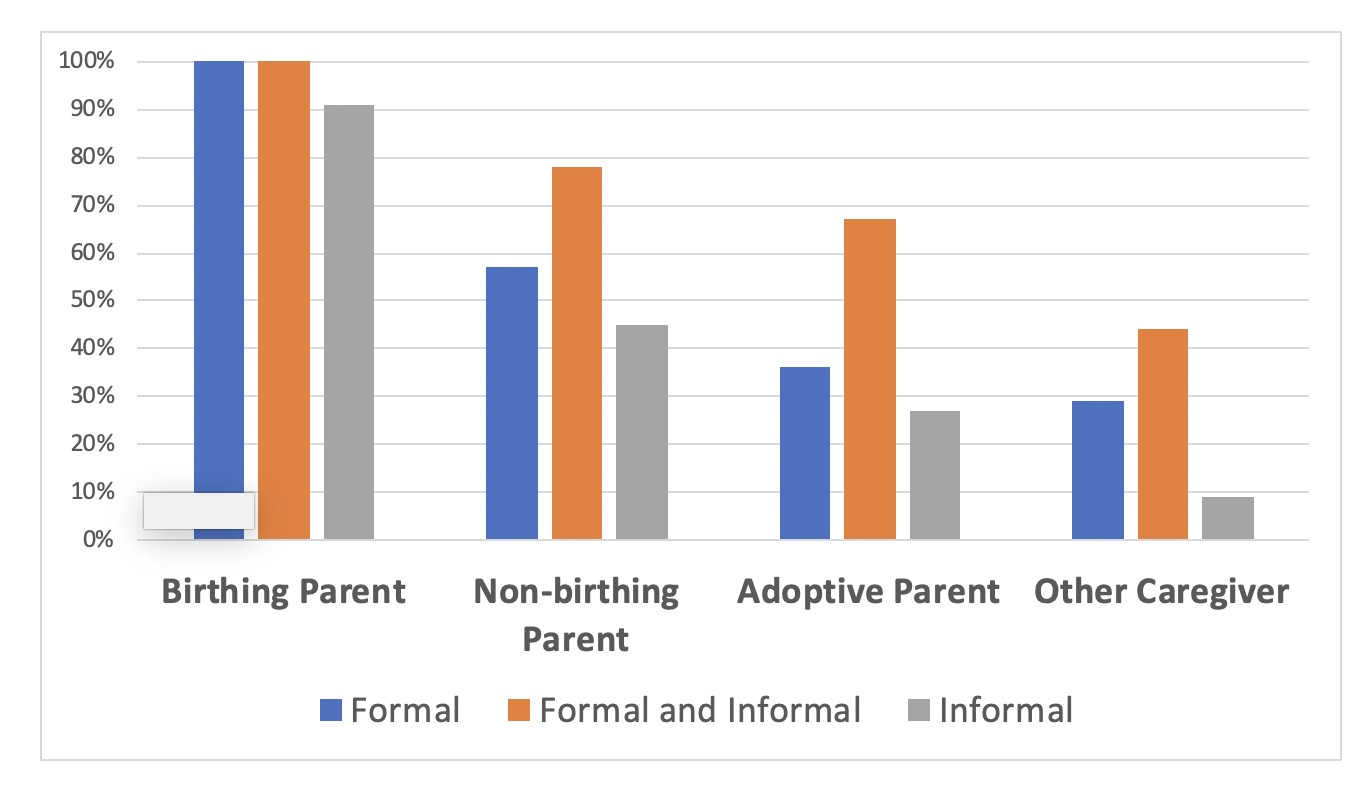
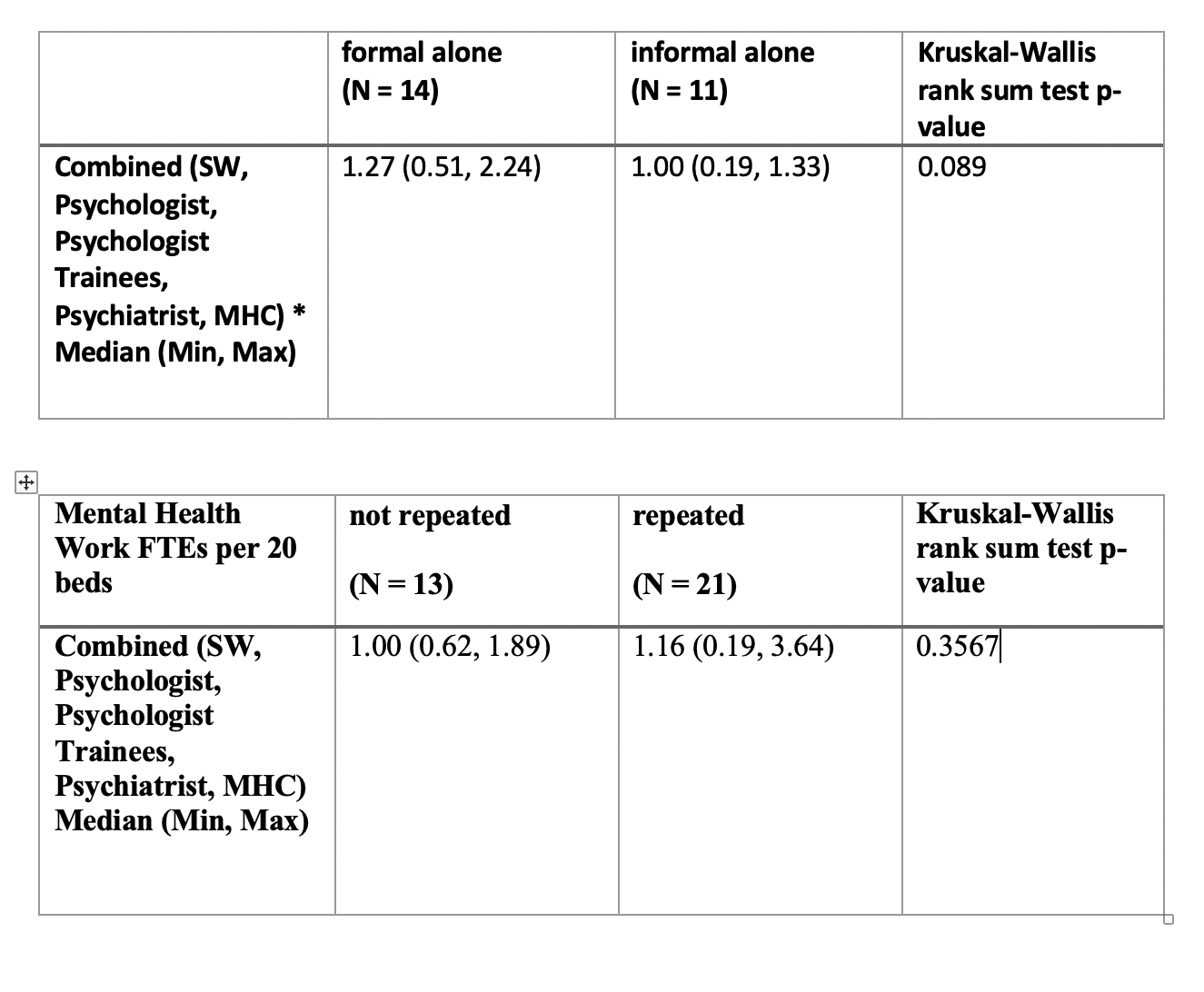
Results: 34 of 44 centers responded. Screening practices vary significantly across centers with 14 centers (41%) performing formal screening only with the birthing parent being the most commonly screened (figure 1). All centers have SW presence, with median ratio of 1:20. Thirteen (38%) centers have NICU-specific psychology support with a median of 0.8 full time equivalents (FTE). Few centers had support from other MHPs (table 1). Centers performing formal screening tended to have higher cumulative MHPs than those performing informal screening (p=0.089). Centers performing repeat screening demonstrated no difference in the number of mental health professionals (p=0.3567) (tables 2 and 3).
Conclusion(s): Despite elevated risk for PMADs in NICU parents, screening practices for mental health disorders are highly variable in CHNC centers, and less than half of centers have dedicated MHPs. Centers that screen formally had more cumulative mental health professionals. Thus, it is likely that creating a sustainable model to adequately detect PMADs will require more MHPs in the NICU.
.png)