Neonatology
Session: Neonatal/Infant Resuscitation 2
273 - Investigating the efficacy of intranasal and endotracheal epinephrine administration in moderately asphyxic newborn lambs.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 273
Publication Number: 273.2930
Publication Number: 273.2930

Graeme Polglase, PhD (he/him/his)
Professor, Deputy Centre Head
The Ritchie Centre, Monash University and Hudson Institute
Melbourne, Victoria, Australia
Presenting Author(s)
Background: Birth Asphyxia is one of the greatest causes of death in children under 5 years, responsible for ~1 million deaths annually. In the most severe cases of asphyxia newborns require chest compressions and adrenaline. While rare, the outcomes are devastating, with high rates of morbidity and mortality. While intravenous adrenaline is the optimal route of administration, it requires surgical implantation of a catheter under sterile conditions which may delay its administration, or not be possible in resource limited settings.
Objective: To investigate the utility of endotracheal or intranasal routes of adrenaline administration as alternatives to intravenous adrenaline in severely asphyxiated newborn lambs.
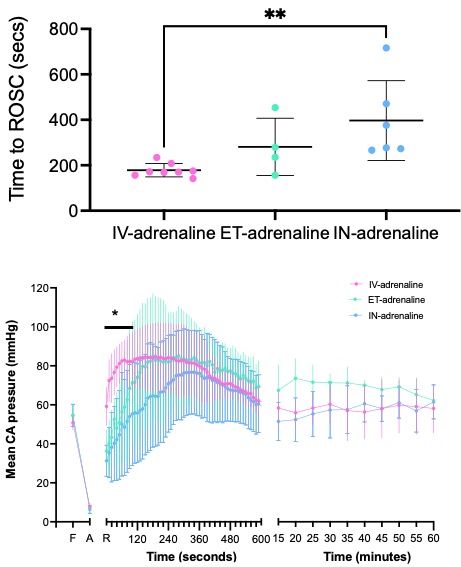
Design/Methods: Near-term fetal lambs of 140 days gestation (term ~148 days) were exposed via caesarean section and catheters and flow probes surgical placed for measurement of pulmonary, systemic and cerebral blood pressures and flows. Asphyxia was induced by cord clamping and delaying resuscitation until blood pressure reached ~9 mmHg and heart rate was < 60 bpm. Lambs were randomised to receive ventilation, chest compressions and either intravenous (0.02 mg/kg, n=8), intranasal (0.1 mg/kg, n=8) or endotracheal (0.1 mg/kg, n=7) adrenaline. The primary outcomes were time to Return of Spontaneous Circulation (ROSC) as well as the overshoot in carotid blood pressure and flow.
Results: 100% of intravenous lambs achieved ROSC while 85% of intranasal and 71% of endotracheal achieved ROSC. Intranasal lambs were significantly slower at attaining ROSC (397±176s) than intravenous lambs (178±30s) while endotracheal lambs were not different to either groups (281±126s). However, intravenous lambs had a rapid overshoot in carotid blood pressure within 90s, while endotracheal (190s) and intranasal (310s) lambs took signficantly longer (p < 0.01). Intravenous lambs had significantly higher carotid blood flow for the first 10 minutes after ROSC compared to endotracheal and intranasal lambs. Blood gas and oxygenation variables were not different between groups. Plasma adrenaline levels were significantly lower in intranasal lambs compared to endotracheal and intravenous adrenaline groups (p < 0.05).
Conclusion(s): In severely asphyxic near-term lambs, intravenous adrenaline is the most superior in achieving ROSC and time to ROSC, however results in a rapid overshoot in carotid blood pressure and flow which may increase the risk of cerebrovascular injury. Endotracheal and intranasal adrenaline had similar rates of ROSC and may be effective alternatives when intravenous administration is delayed or not possible.