Neonatology
Session: Neonatal Neurology 5: Clinical
537 - White Matter Injury on Early versus Term-equivalent Age Brain MRI in Infants Born Very Preterm
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 537
Publication Number: 537.1222
Publication Number: 537.1222

Sriya Roychaudhuri, MD, MRCPCH (she/her/hers)
Clinical Assistant Professor
University of British Columbia Faculty of Medicine
Vancouver, British Columbia, Canada
Presenting Author(s)
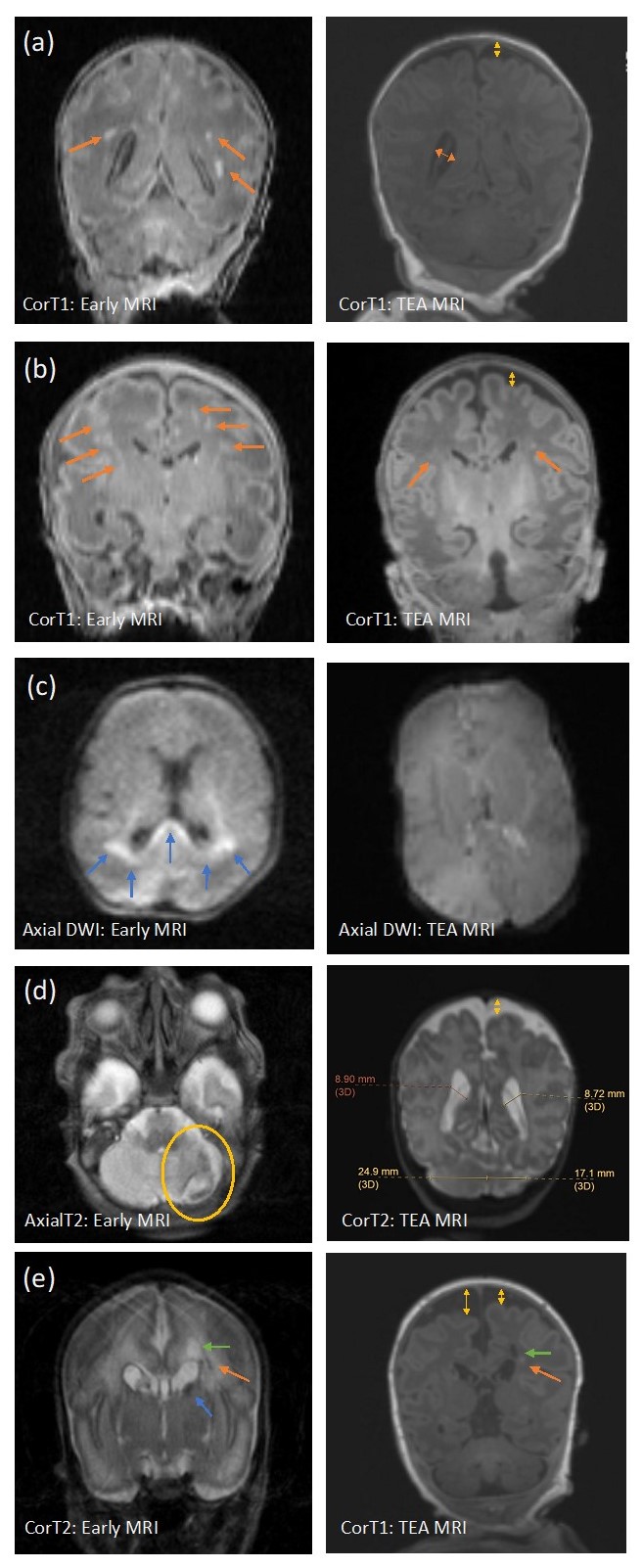
Background: White matter injury (WMI) in infants born preterm is the most prevalent form of injury and associated with adverse neurodevelopmental outcomes. Magnetic resonance imaging (MRI) has distinct advantages over routine cranial ultrasound to visualize WMI in the initial weeks following preterm birth and at term-equivalent age (TEA). Systematic MRI scoring methods to assess the extent of WMI have been proposed for both early and TEA times. Early MRI interpretation focuses on characterization of the number and size of the WMI lesions, whereas TEA MRI captures sequelae of prior injury such as cystic lesions, signal abnormalities, delayed myelination and white matter volume loss.
Objective: To compare WMI on early brain MRI, at 30 to 34 weeks post-menstrual age (PMA), with WMI assessment at TEA (37-42 weeks PMA) MRI, using two standardized scoring systems, in infants born < 33 weeks gestational age (GA).
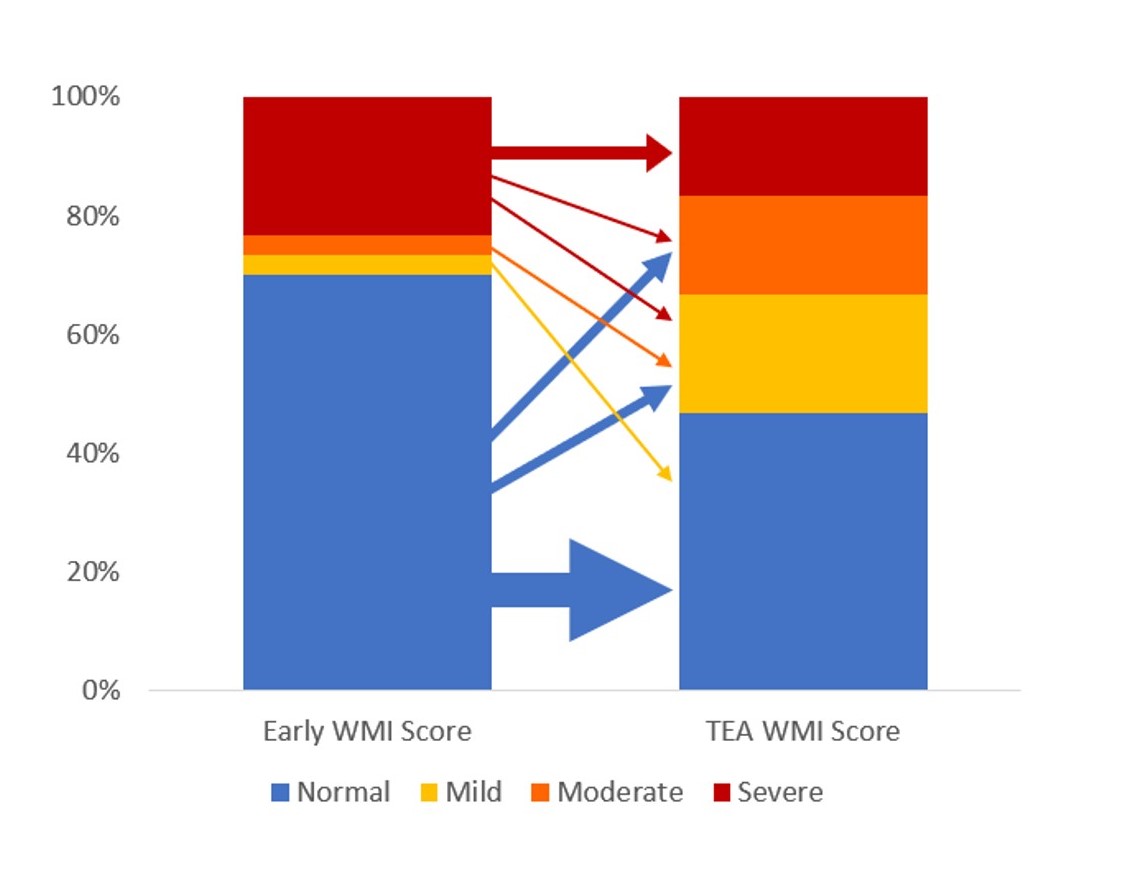
Design/Methods: The Miller et al scoring was used for categorization of injury on early MRI. TEA MRIs were assessed for WMI and its sequelae using the Kidokoro et al score. The degree of WMI and global injury were categorized as normal-mild and moderate-severe. Global injury scores consider presence and degree of intraventricular hemorrhage and ventricular dilation along with WMI. We assessed the relationship between early and TEA classifications using Fisher’s exact tests.
Results: The cohort consisted of 30 infants with mean GA of 28.7 weeks and median birthweight of 1220 grams. The early MRIs were performed at an average of 33.0 weeks (SD = 1.4), and the TEA MRIs at 38.6 weeks (SD = 1.4) PMA (Figure 1). There was a strong association between the systematic assessments of global injury severity (p < 0.001) and WMI (p=0.007) at the two time points (Table 1)(Figure 2). There was no instance of newly detected WMI or increased lesion severity noted on TEA when compared to early MRI scans.
Conclusion(s): Evaluating brain injury using standardized scoring systems enables clinicians and researchers to analyze images in a systematic manner and follow WMI longitudinally in very preterm infants. Although the optimal timing to undertake neuroimaging in the preterm infant remains to be determined, early (30-34 weeks) and TEA MRI may independently provide valuable information on WMI and risk for associated sequelae.
.jpg)