Neonatology
Session: Neonatal Neurology 3: Clinical
35 - Acuity of brain injury is associated with early blood glucose trajectory in neonates with hypoxic-ischemic encephalopathy
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 35
Publication Number: 35.548
Publication Number: 35.548

Thomas R. Wood, MD, PhD (he/him/his)
Assistant Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: Early glucose abnormalities are associated with brain injury and worse outcomes in neonatal hypoxic-ischemic encephalopathy (HIE). Glycemic state may differ by chronicity of injury: hyperglycemia may reflect decreased glucose utilization in acute injury and hypoglycemia may be the result of depleted fetal glucose stores in indolent/subacute injuries.
Objective: We hypothesize that glucose aberrations within the first 24 hours of birth are associated with acuity of brain injury on MRI in neonates with HIE.
Design/Methods: This is a post-hoc analysis of the High-dose Erythropoietin for Asphyxia and Encephalopathy Trial. Infants with blood glucose (BG) values recorded within 24h and MRI within 4-7 days of birth were included. Hypoglycemia, euglycemia, and hyperglycemia were defined as BG < 50 mg/dL, BG 50-200 mg/d, and BG >200mg/dL, respectively. Chronicity of injury on MRI was categorized by 3 experienced reviewers as normal (no signal abnormalities on diffusion, T1/T2 imaging), acute (restricted diffusion alone), subacute (abnormal T1/T2 without corresponding diffusion changes), and acute+subacute (restricted diffusion and T1/T2 changes in different regions). Linear regression models with robust standard errors comparing glucose profile by chronicity of injury were adjusted for HIE severity, hydrocortisone/inotrope use 1st day, small or large for gestational age, intubation, 10 min Apgar, and Epo vs. placebo treatment.
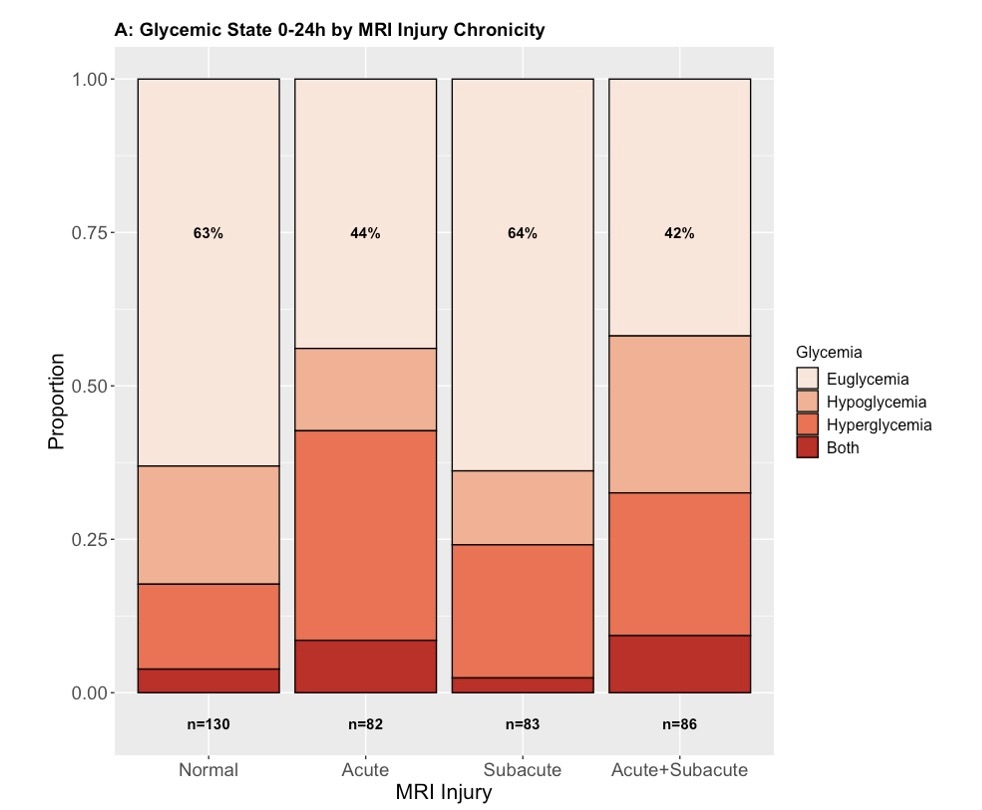
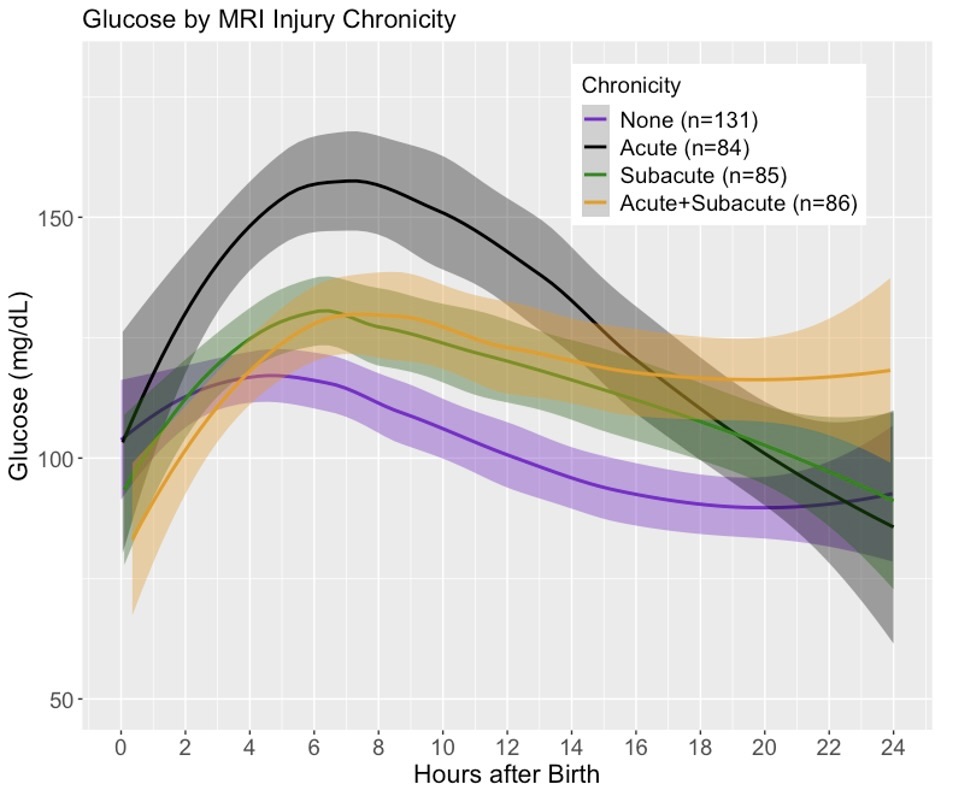
Results: 381 infants (male 55%; mean (SD) gestational age 39.1 (1.4) weeks; 3,138 BG values) were included in the analysis. There were 130 (34%) normal MRIs, 82 (22%) acute, 83 (22%) subacute, and 86 (23%) acute+subacute injuries. The proportion of euglycemic infants differed by injury and chronicity – no injury (63%), acute (44%), subacute (64%), acute+subacute (44%) (p=0.012, Fig 1). Infants with acute injury had the highest proportion of hyperglycemic BG values (34%). Infants with subacute injury had lower BG after birth compared to those with no injury, and all infants with injury displayed a sharp early increase in BG that peaked at 6-8h after birth (Fig 2). In the first 2h, infants with acute+subacute injury had significantly lower minimum BG compared to those with normal MRI (-29.4 mg/dL, 95% CI -50.1, -8.7; p=0.006, Fig 3A). Across the first 24h, infants with acute injury had a significantly higher maximum BG compared to normal MRI (+24 mg/dL, 95% CI 2.5, 45.5; p=0.029, Fig 3B).
Conclusion(s): Infants with HIE display distinct glycemic patterns based on their chronicity of injury, supporting the hypothesis that timing of injury affects early glucose metabolism.
.jpg)
