Emergency Medicine
Session: Emergency Medicine 4: Infections
103 - Impact of the amount of intravenous glucose administration on hospitalization for acute gastroenteritis in a pediatric emergency department.
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 103
Publication Number: 103.1580
Publication Number: 103.1580

Jocelyn Gravel, MD, MSc (he/him/his)
Attending
CHU Sainte-Justine
Montreal, Quebec, Canada
Presenting Author(s)
Background: In case of failure of oral rehydration, children with acute gastroenteritis can be hydrated using intravenous (IV) solution. The choice of the IV solution itself (solutions containing dextrose versus crystalloids alone) and the glucose quantities to administer are not well established.
Objective: The main objective of this study was to evaluate the impact of the amount of IV glucose provided to children treated for acute gastroenteritis on hospitalizations. Other objective was to evaluate practice variation regarding the amount of glucose provided for IV rehydration in a pediatric emergency department (ED).
Design/Methods: We conducted a retrospective cohort study from 2019-2022 in a Canadian pediatric ED. We included children with acute gastroenteritis undergoing IV rehydration. Patient with hypoglycemia, metabolic disease or diabetes were excluded. The IV glucose administered during the initial four hours of rehydration was quantified. The primary outcome was hospitalization and return visit in the following 7 days was a secondary outcome. 10% of the charts were evaluated in duplicate to assess inter-rater reliability. We examined glucose infusion distribution at one and four hours, and utilized multiple logistic regression to relate glucose amounts with hospitalization and second visit, accounting for age, weight, bicarbonate levels, ondansetron use, and amount of liquid infused. It was estimated that the evaluation of 250 cases would yield 50 admissions.
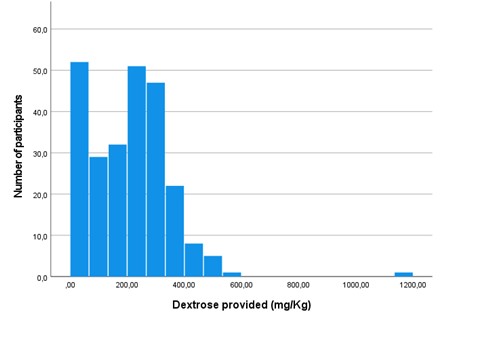
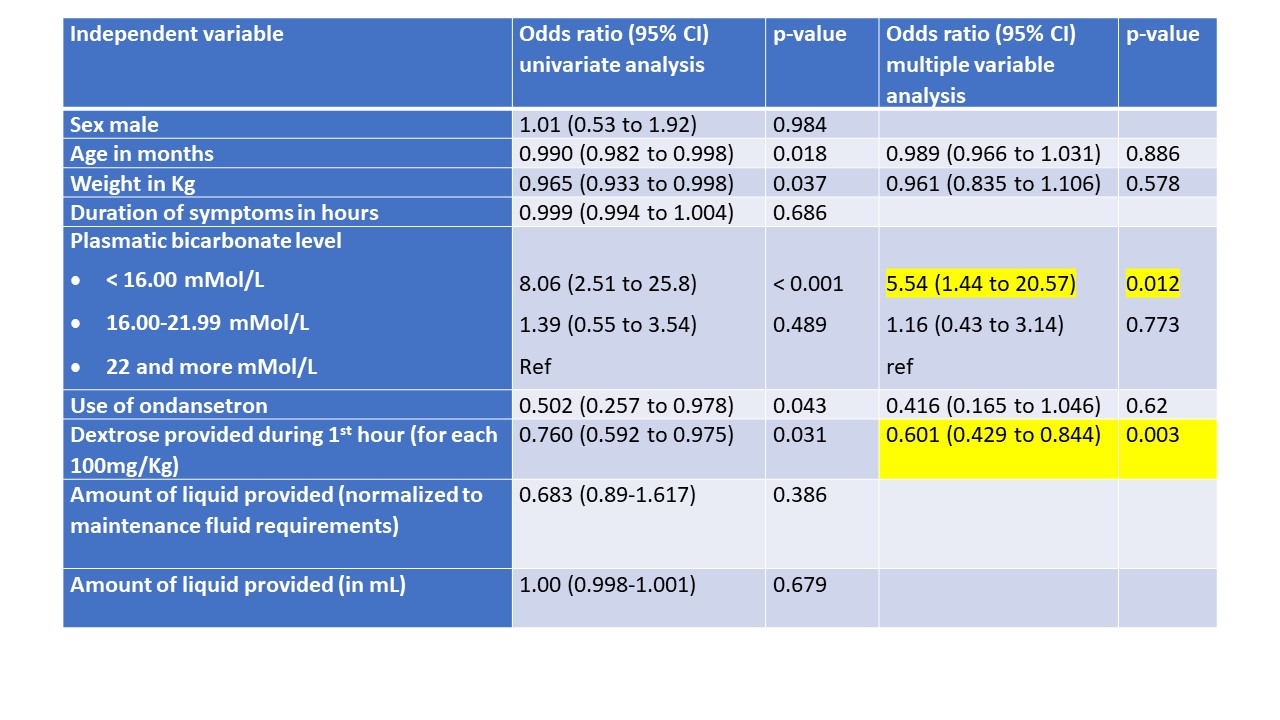
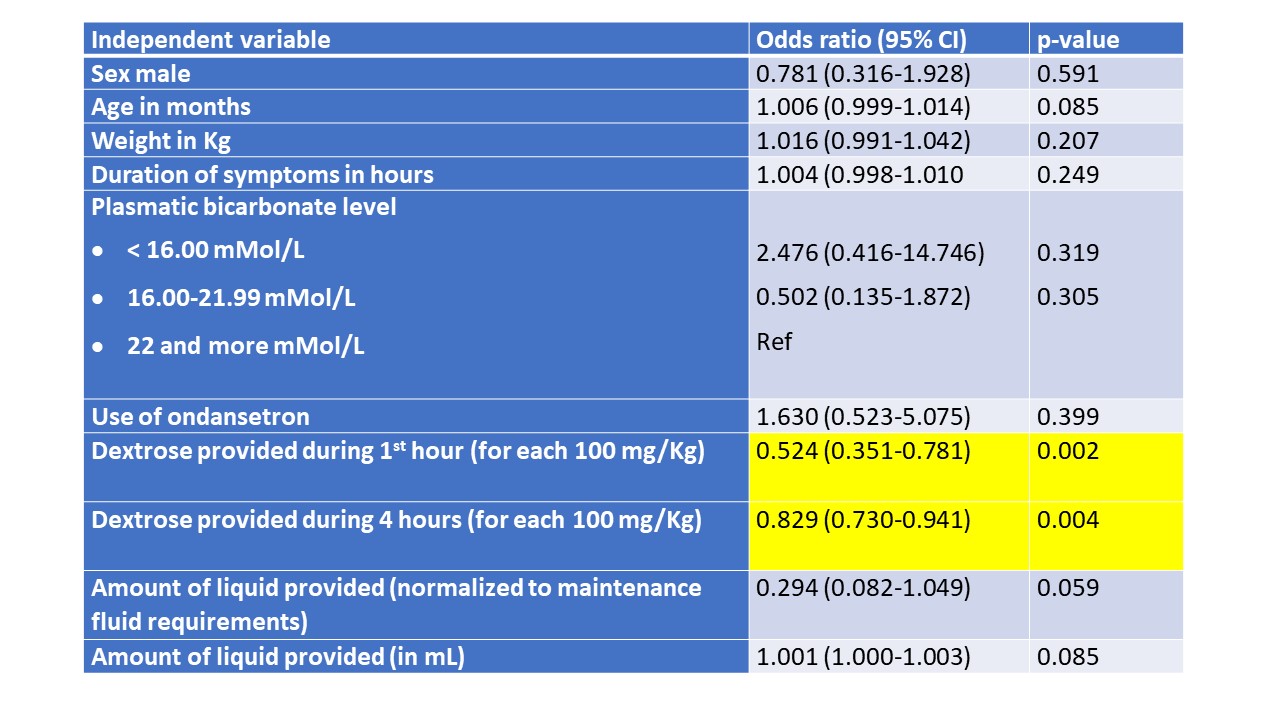
Results: Among 6,939 children evaluated for potential acute gastroenteritis, 250 met our inclusion/exclusion criteria. All variables included in the analysis had excellent inter-rater reliability. Notable variations existed in glucose quantities provided, both at one hour (first quartile: 87 mg/Kg; third quartile: 294 mg/Kg) and four hours (first quartile: 681 mg/Kg; third quartile: 1174 mg/kg) of rehydration. Multiple logistic regression showed a greater hospitalization risk with smaller amount of glucose administered during the initial hour (OR for each 100mg/kg increment: 0.60; 95%CI: 0.42-0.84) and four hours (OR: 0.76; 95%CI: 0.63-0.91) of rehydration. Moreover, children who received more dextrose during the first hour of rehydration were at lower risk of return visit (OR for each 100mg/kg increment: 0.52; 95%CI: 0.35-0.78), as well as during the first four hours (OR: 0.83; 95%CI: 0.73-0.94).
Conclusion(s): There was a wide practice variation in IV glucose provided to children with acute gastroenteritis. In this population, higher IV glucose amount was associated to a lower risk of hospitalization and lower risk of return visit.