Health Services Research
Session: Health Services Research 1: Workforce
283 - Trends in pediatric visits with Pediatricians versus Family Physicians from 1993 to 2019
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 283
Publication Number: 283.1539
Publication Number: 283.1539
- EG
Emily F. Gregory, MD, MHS (she/her/hers)
Assistant Professor
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Physicians in both Pediatrics and Family Medicine care for infants and young children but have demonstrated differences in attitudes towards elements of preventive care and practice patterns. Prior work indicates increasing reliance on Pediatricians to deliver pediatric care in the US through 2006.
Objective: Assess trends in which physicians deliver care to children in the US beyond 2006, and how sociodemographic factors are associated with care patterns.
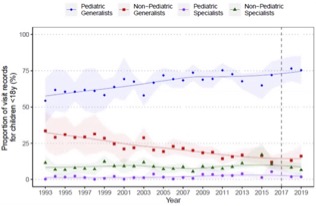
Design/Methods: This cohort study used National Ambulatory Medical Care Survey (NAMCS) data from 1993 - 2019. NAMCS provides estimates of US physician office visits via complex sampling and weighting. We included non-surgical visits for individuals < 18 years. Physician specialty was available from 1993 – 2017. For 2018 – 2019 specialty was inferred from the age mix of patients (>=95% of visits for children < 18 years classified as pediatricians). We assessed trends in the full sample and the subgroup of infants < 1 year using the Mann-Kendall test of trends. We used logistic regression of data from 1997 – 2016 to assess whether race, ethnicity, site of visit (urban versus rural), or payer were associated with odds of pediatrician visits. Regression was limited because of payer coding changes at other time points. Regression also adjusted for time. We applied sample weights to all analyses.
Results: From 1993 – 2019 the proportion of visits to general pediatricians by children aged 0-17 rose from 55% to 75% (Mann-Kendall p-value < 0.01), continuing the trend previously reported through 2006. Meanwhile, the proportion of pediatric visits to family physicians declined from 34% to 16% (Mann-Kendall p-value < 0.01). Similar trends were seen for infants < 1 year. Regression demonstrated increased odds of Pediatric visits (versus Family Medicine) for visits for children with Black race compared to non-Black race (OR 1.5, 95% CI 1.2 – 1.9) or Hispanic ethnicity compared to non-Hispanic ethnicity (OR 1.3, 95% CI 1.0 – 1.7) and decreased odds of visits to Pediatrics in rural areas (OR 0.3, 95% CI 0.25– 0.43). Payer was not associated with change in odds of visits to Pediatricians.
Conclusion(s): We found continued increasing reliance on Pediatricians to deliver pediatric care, particularly in urban areas and for Black and Hispanic children. This has implications for multiple aspects of health care delivery, including the need for enhanced pediatric exposure for rural family medicine physicians and increased exposure for pediatricians to aspects of adult care relevant to child and family health, such as tobacco use or social determinants of health.