Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 1: PDA
78 - Use of Automated Photoplethysmography to Detect Symptomatic Patent Ductus Arteriosus
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 78
Publication Number: 78.1890
Publication Number: 78.1890

Ignacio J. Contreras, MD (he/him/his)
Fellow
Cohen Children's Medical Center
Bayside, New York, United States
Presenting Author(s)
Background: Photoplethysmography (PPG) employs non-invasive, electro-optic technology to monitor and detect changes in blood volume in peripheral blood vessels. Using manual analyses of PPG wave forms, we have previously shown that pre- and post-ductal pulse transit times (PTT) correlate with cardiac stroke volume (SV). Symptomatic PDA (sPDA) in preterm infants is characterized by markedly elevated SV. Automation of PPG analysis may enable rapid diagnosis of sPDA at the bedside, which could facilitate medical treatment and further interventions.
Objective: Our objectives are to: 1) compare automatic PPG measurements of PTT relative to manual, 2) determine whether PTT correlates with SV in infants, and 3) compare PTT before and after closure of sPDA.
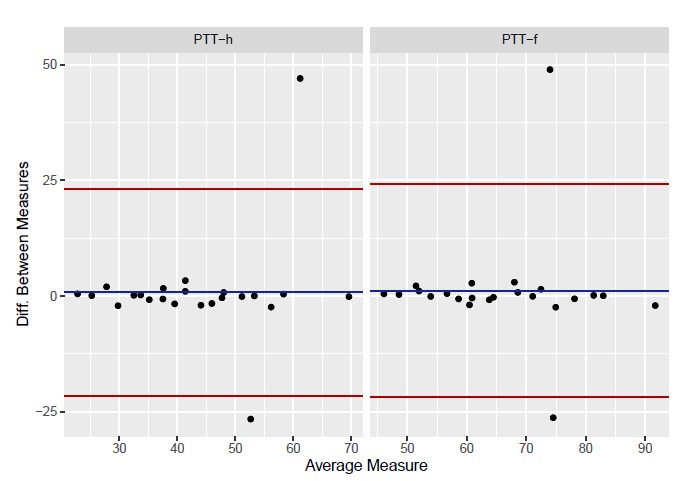
Design/Methods: Pulse oximetry probes for PPG were placed on the right hand and either foot of 15 preterm neonates before and after transcatheter PDA closure (Piccolo, Abbott Cardiovascular, Plymouth, MN). All infants had sPDA before closure, and no ductal flow after closure, confirmed by echocardiography. PTT were calculated from the start of the R wave of the ECG to the maxima of the waveforms of the hand and foot both manually and by using the automated PPG (Lev Academic Center, Jerusalem, Israel). All calculations were based on the mean of the means of two epochs. Manual and automated PPG parameters were compared using Bland-Altman analysis. Echocardiographic measurements of SV before and after sPDA closure were compared by paired t-test, and correlations with PTT by Pearson’s product moment coefficient. PTT before and after sPDA closure were compared using paired t-tests.
Results: Manual and automated PTT measurements were well correlated (Figure 1). SV decreased after sPDA closure as expected, from 3.37+/-1.55 to 2.76+/-0.85 ml (p=0.27). PTT correlated with SV in both the hand (r=0.767, p=0.010) and foot (r=0.814, p=0.004) before sPDA closure, but only in the hand after closure (r=0.650, p=0.022). PTT increased significantly after PDA closure in both the hand (35.34+/-9.43 ms to 49.25+/-10.3 ms) and foot (60.92+/-10.33 ms to 70.79+/-13.22 ms) (p < 0.005).
Conclusion(s): Automated PPG waveform analysis provides PTT that are statistically identical to manual measurements. PTT is rapid in infants with sPDA, likely because of decreased vascular compliance related to increased SV. Automated PPG assessments of PTT may be a feasible tool for detecting sPDA in real time.