Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 3
470 - Antenatal Counselling for Anticipated Preterm Birth at the Limits of Viability in Non-Tertiary Centers: How Can it be Improved?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 470
Publication Number: 470.3202
Publication Number: 470.3202

Alessia Gallipoli, MD, MHSc
Neonatologist & Fellow in Neonatal-Perinatal Ethics
Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Presentations of preterm labour < 25 weeks gestational age (GA) to non-tertiary centres require timely evidenced-based counselling to facilitate informed decision making and optimize management and outcomes. Variation in how counselling is provided in these centres can impact management decisions and the resultant short- and long-term outcomes for infants and families.
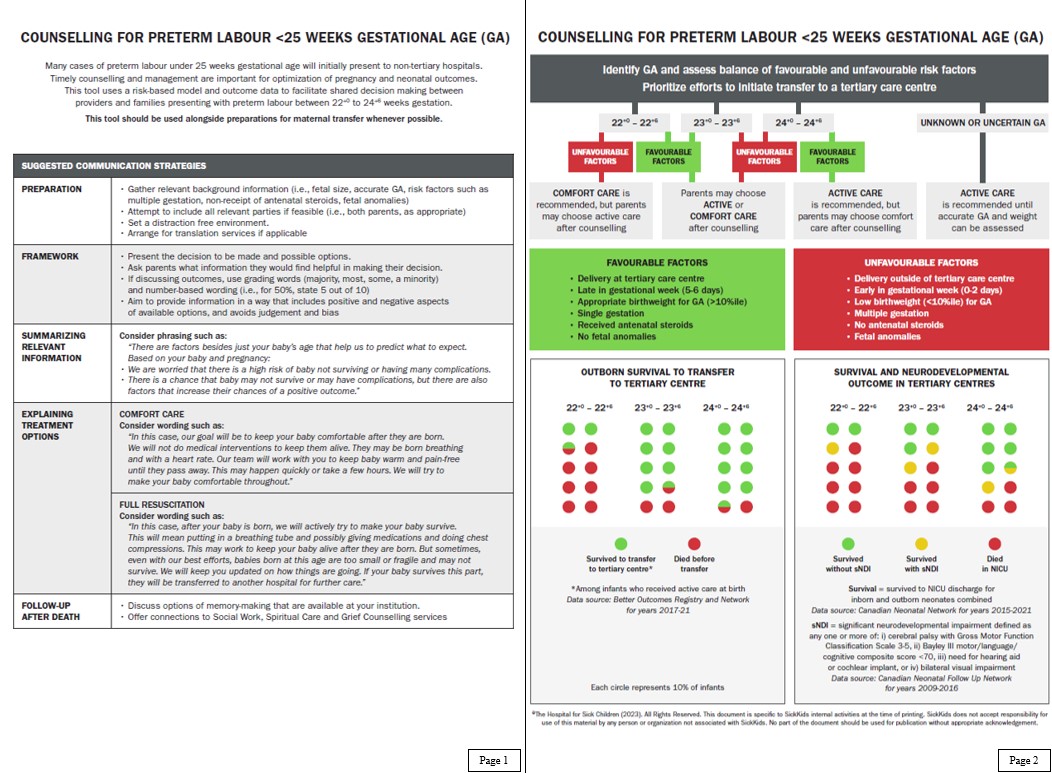
Objective: (1) To develop a visual counselling tool that incorporates risk-based modifiers and local outcome data to support counselling for preterm birth at < 25 weeks GA in non-tertiary centres and (2) To refine and facilitate utilization of this tool through the development of an understanding of the barriers and challenges to providing counselling and care at periviable GAs in these centres.
Design/Methods: Perinatal risk factors and local outcome data were incorporated into a visual counselling tool. Semi-structured interviews were conducted with participants with experience in providing or receiving care at < 25 weeks GA in non-tertiary centres. Interviewees included transport team members, paediatricians, obstetricians, one family physician and one parent. Analysis using interpretive description qualitative methodology was performed to identify themes in the practice and experience of participants.
Results: A two-page counselling tool was developed, including a risk-based decision algorithm with local outcome data, along with guidance for carrying-out counselling discussions. Twenty-one interviews were completed to identify themes in participant experiences and assist in facilitating utilization of this tool. Barriers to counselling identified include lack of updated knowledge on resuscitation practices in tertiary centres, discomfort in providing counselling, variability in counselling content, and variation in health care provider (HCP) teams involved in counselling. All HCPs expressed desire for further education in this area.
Conclusion(s): Support for HCPs in non-tertiary centres in the counselling of periviable preterm families is much needed. The development of our practice tool targeted for non-tertiary centres provides an important step in this process. Next steps include mounting a response to the expressed need from HCPs for expanded and targeted education and training in the counselling and management of periviable preterm pregnancies.