Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
184 - Bronchopulmonary dysplasia in extreme preterms: does the definition matter?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 184
Publication Number: 184.3119
Publication Number: 184.3119

Sophie Piedboeuf, MD (she/her/hers)
Pediatric Resident, PGY-3
Faculty of Medicine Université Laval
Québec, Quebec, Canada
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is the most prevalent complication of extreme preterm birth and a well-established risk factor for long-term adverse outcomes. Yet, there are variations in its clinical definition which may have important implications for research, benchmarking, and quality improvement of care.
Objective: To evaluate the impact of BPD definitions on 1) the estimated incidence of BPD and 2) rankings of neonatal intensive care units (NICUs) for benchmarking.
Design/Methods: Secondary analysis of the MOBYDIck (NCT02371460) randomized, placebo-controlled trial conducted in infants born < 29 weeks of gestation from 16 Canadian NICUs between 2015 and 2018. This trial investigated the effect of maternal docosahexaenoic acid on survival without BPD at 36 weeks’ corrected age. BPD (and grading) based on assessment at 36 weeks’ corrected age were classified according to CNN, NICHD 2018 and NRN 2019 definitions alone and in combination to a supplemental oxygen reduction test (SORT). Definitions were compared in the entire cohort using the weighted kappa coefficient (WK). For NICUs comparison, units with less than 30 infants were regrouped in one composite unit and BPD was considered present only if categorized as moderate or severe.
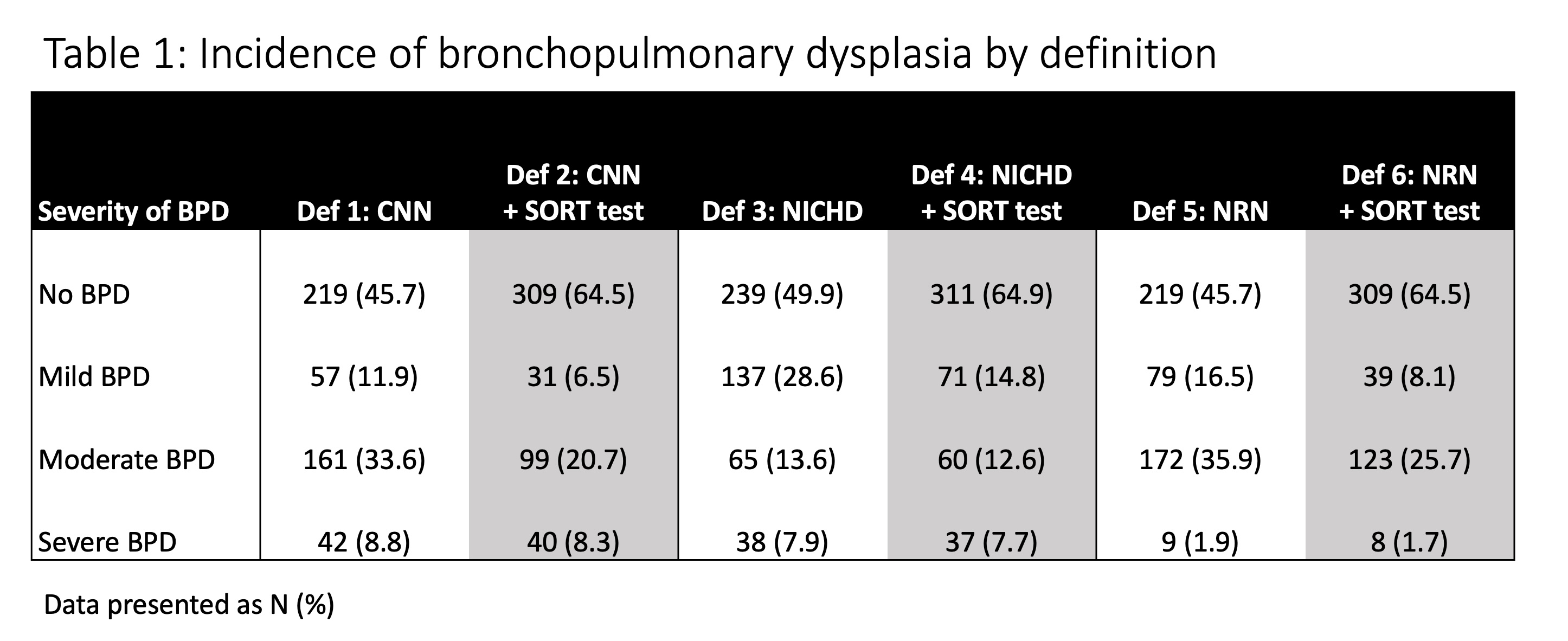
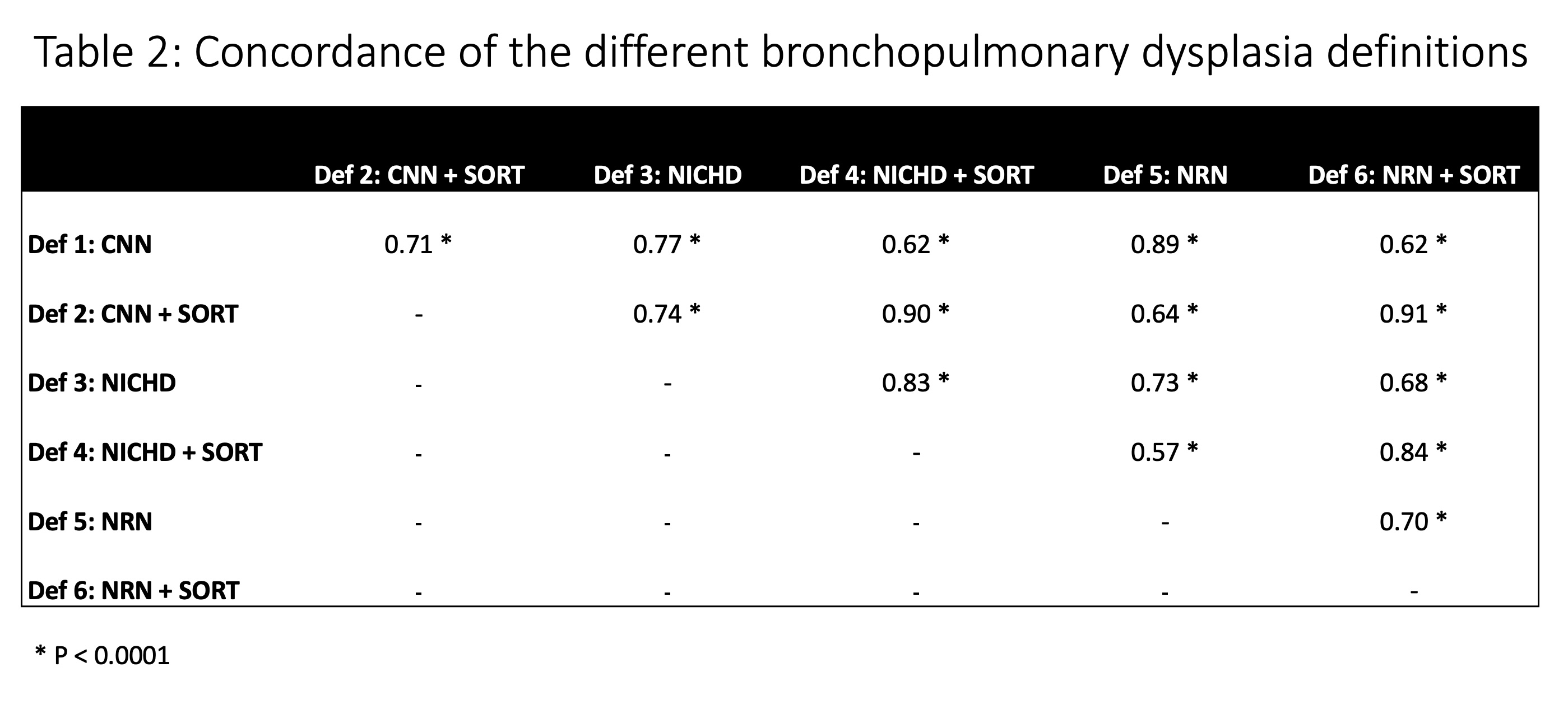
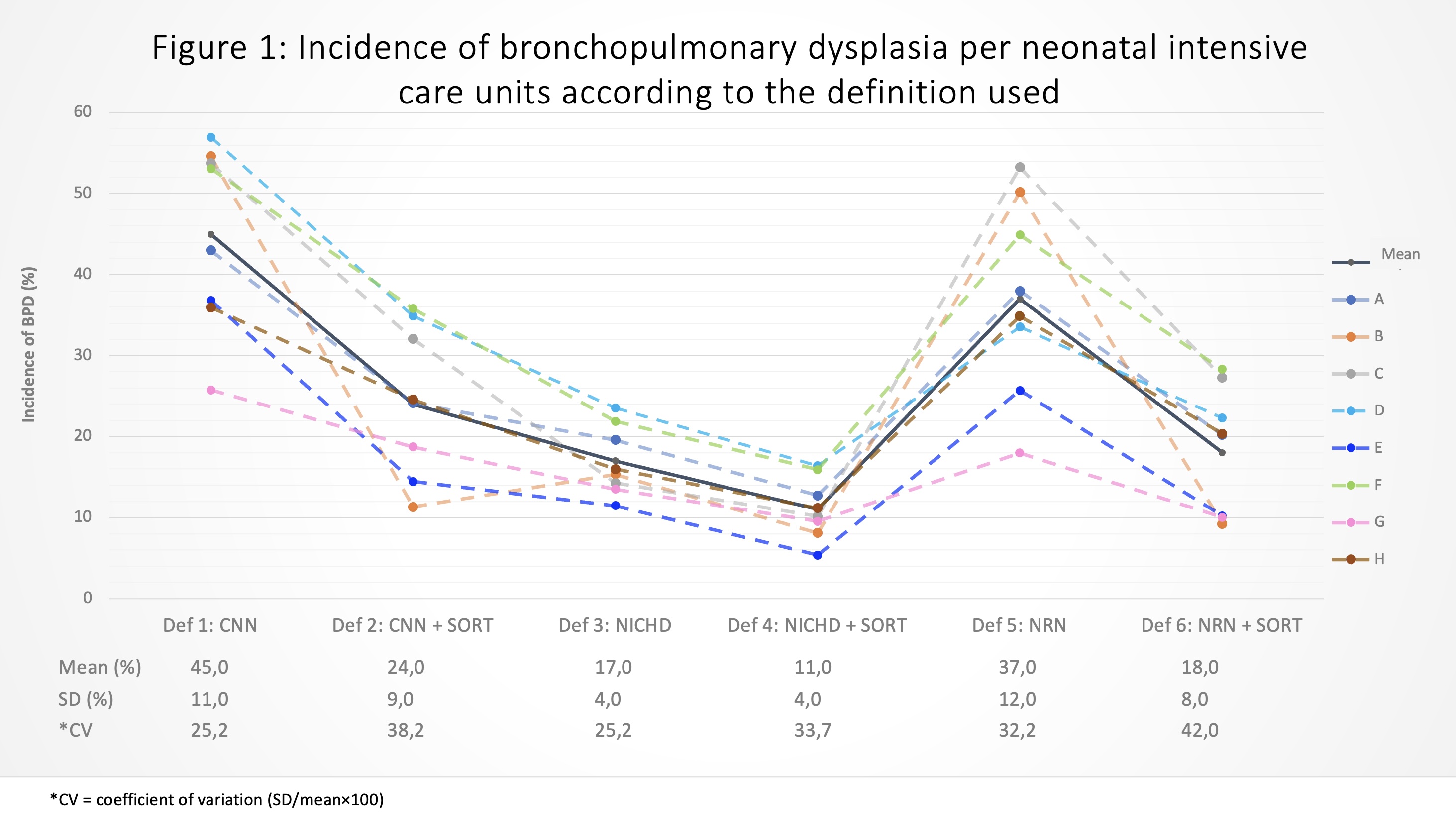
Results: Data to classify BPD according to the 6 definitions was available in 479/523 (91.6%) infants included in the original trial (mean gestational age 26.7 weeks, SD 1.5; 221 males, 52.5%). Important variations in the rate and severity of BPD were noted according to the definition used. As seen in Table 1, including the SORT to each definition significantly lowered the rate of BPD: CNN 54.3% vs 35.5%; NICHD 50.1% vs 35.1%; NRN 54.3% vs 35.5% while having minimal impact on severe BPD. Table 2 shows that the definitions correlate only moderately but including the SORT increased the correlation: for CNN compared with NICHD, WK increased from 0.77 [CI 0.62-0.72] without SORT to 0.90 [IC 0.87 à 0.93] with SORT. The magnitude of the changes for BPD incidence and units’ ranking (out of 8) were important for some NICUs (Figure 1). Including the SORT to the NICHD definition caused a lesser change in BPD incidence and units ranking compared to CNN and NRN. The coefficient of variation (CV) between 25 and 42% demonstrates the clinical significance of the change in ranking.
Conclusion(s): The choice of BPD definition can lead to significant changes in population estimate, resulting in important variation in the ranking of units. This can impact benchmarking and research. Future studies should evaluate the predictive value of those definitions on long-term adverse outcomes.