Neonatology
Session: Neonatal/Infant Resuscitation 1
259 - Evaluation of respiratory patterns at birth of preterm infants assisted in the delivery room with two different levels of static CPAP: single-center retrospective study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 259
Publication Number: 259.3070
Publication Number: 259.3070

Francesco Cavigioli, MD (he/him/his)
Neonatologist
NICU, Buzzi Children's Hospital ASST FBF Sacco
V.Buzzi Children's Hospital, ASST-FBF-Sacco
Milan, Lombardia, Italy
Presenting Author(s)
Background: There is much debate about the optimal positive pressure level to be delivered to premature infants with adequate spontaneous respiratory drive to facilitate the cardio-respiratory transition at birth. Recent European guidelines for the management of neonatal RDS suggest using an initial CPAP with a pressure of at least 6 cmH2O; however, about 50% of premature infants see failure of noninvasive respiratory support within the first 5 days of life.
Objective: To evaluate the impact of two static CPAP levels on respiratory patterns and other ventilatory and oxygenation parameters in a population of preterm infants in the delivery room
Design/Methods: Single-center study of preterm infants between 26 and 29+6 weeks' gestation, spontaneously breathing, supported with face mask and T-piece with two different levels of CPAP (5 or 8 cmH2O), for respiratory distress at birth. With a respiratory function monitor (RFM), delivered pressures, tidal volumes (Vt), oxygen saturation (SpO2), heart rate (HR), fraction of inspired oxygen (FiO2) and respiratory patterns were recorded.
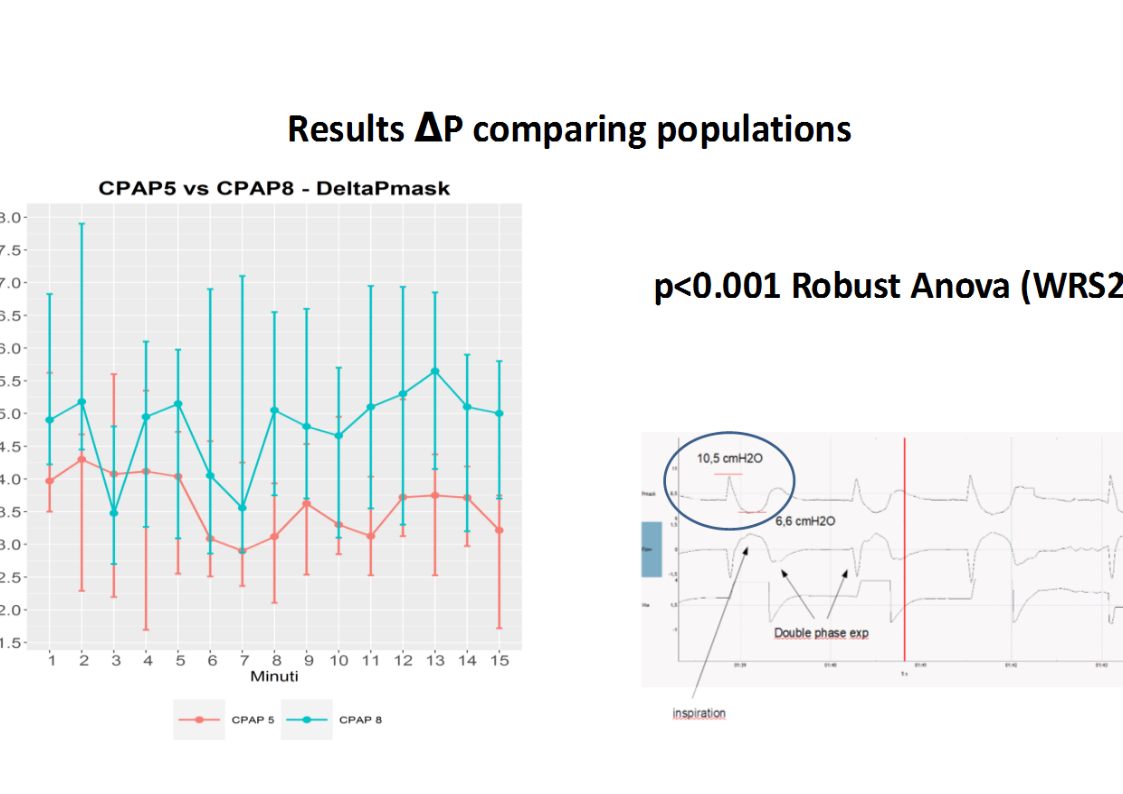
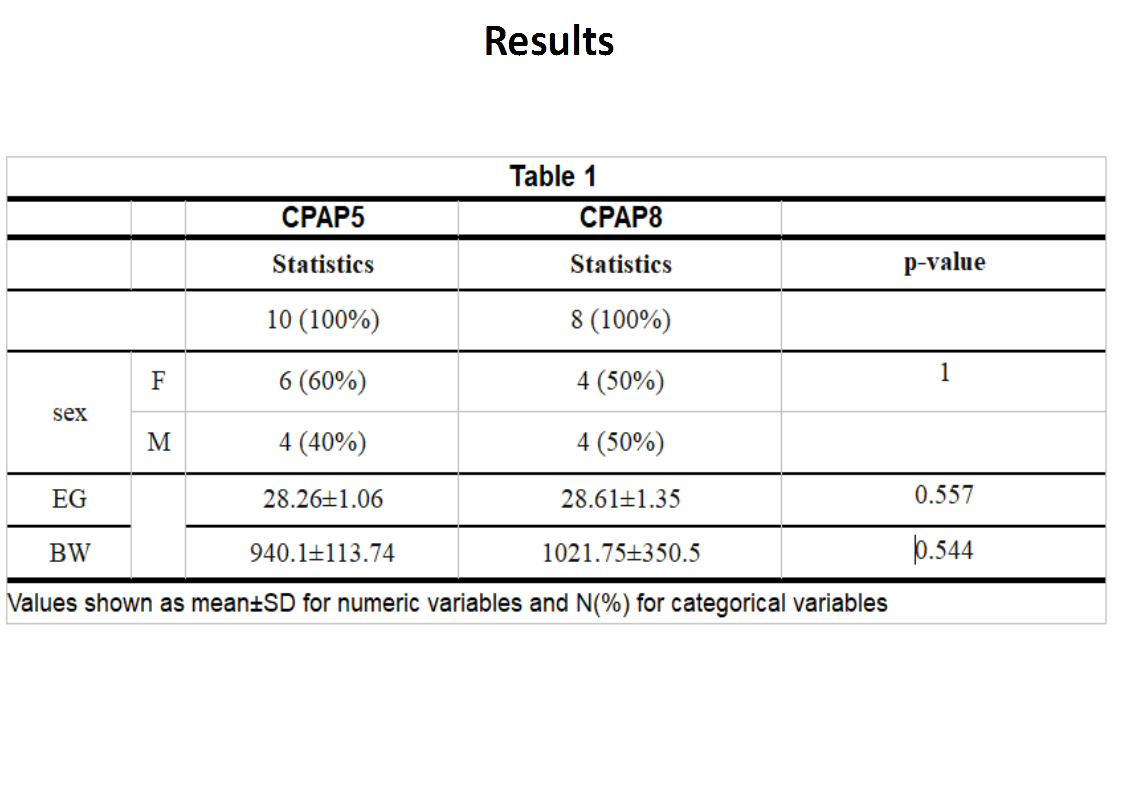
Results: RFM records of 18 infants spontaneously breathing on CPAP delivered by face mask (10 received CPAP of 8 cmH2O and 8 received CPAP of 5 cmH2O) were analyzed. The two levels of CPAP provided good cardiorespiratory adaptation in terms of heart rate (HR) and oxygen saturation (SpO2) in all infants. However, in both groups, there was a transient but significant reduction in HR (p-value=0.02) and SpO2 (p-value < 0.001) in the first few minutes to be attributed to an elicitation of the trigeminal-cardiac reflex from facial compression with the mask. Respiratory pattern 1 (expiratory hold with single expiratory phase) was prevalent in CPAP 5 group and pattern 2 (expiratory hold with multiple expiratory phase) in CPAP 8 group. The CPAP 8 group had lower exhaled tidal volumes, longer expiratory times with lower I:E ratios, and higher delta-pressure in the CPAP level during the spontaneous breathing cycle.
Conclusion(s): The administration of different CPAP levels with T-piece and face mask impacts on breathing patterns of the preterm newborn at birth. Differences could be related to either more prolonged glottis closure during expiratory phase or higher intrinsic work of breathing with the higher CPAP level, which could affect short and medium term outcomes. Future studies comparing different devices to deliver CPAP (e.g., T-piece, r-PAP,etc), as well as different levels of static or dynamic CPAP, may be useful to provide additional data related to the fetal-neonatal cardio-respiratory transition phase.
.png)