Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 1: PDA
79 - Predictive Modeling Using Continuous Vital Sign Monitoring Can Identify a Hemodynamically Significant Patent Ductus Arteriosus in Preterm Neonates
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 79
Publication Number: 79.1928
Publication Number: 79.1928

Amy A. Hobson, DO (she/her/hers)
Neonatology Fellow Physician
University of Iowa Stead Family Children's Hospital
Iowa City, Iowa, United States
Presenting Author(s)
Background: Premature infants are at increased risk for complications from a hemodynamically significant patent ductus arteriosus (hsPDA). Clinical signs of a high-volume PDA shunt are imprecise, which may lead to delays in disease recognition and therapeutic intervention. The use of predictive modeling, based on continuous vital sign monitoring, to enable earlier detection of higher volume shunts represents a knowledge gap.
Objective: To create a clinical model to predict presence or severity of a hsPDA in premature infants.
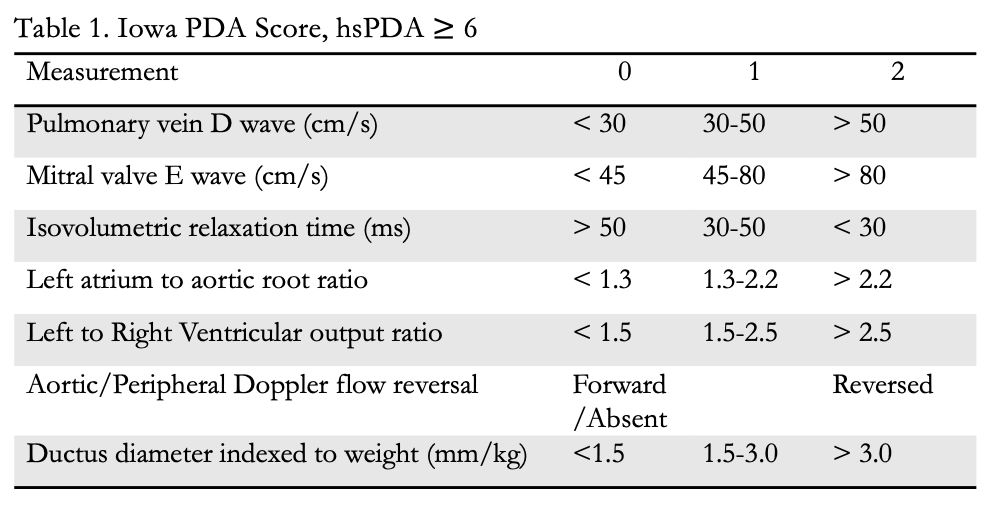
Design/Methods: A retrospective cohort analysis of infants < 27 weeks gestational age from 3/20-9/23 who underwent targeted neonatal echocardiography (TnECHO) screening for hsPDA was conducted at the University of Iowa. TnECHOs were categorized as high-volume PDA (score ≥ 10) or no PDA based on Iowa PDA score (Table 1). Continuous vital sign data including postductal arterial waveform were collected and evaluated in 5-minute increments for the hour preceding each TnECHO. For each increment, a Fourier transform was applied to the arterial blood pressure waveform to obtain the values of the first through fourth harmonics, as well as the ratio of the slope between harmonics 1 and 3 to the slope between harmonics 2 and 4. The percentage of the cardiac cycle was calculated to obtain the blood pressure (BP) less than 80% of the mean over the cycle, and the standard deviation of the systolic and diastolic BPs over the 5-minute increment. The predictor variables included heart rate, mean BP indexed to heart rate, pulse pressure, weight, postnatal age, gestational age and those above derived from the waveform. These were used to create a logistic regression model to classify each 5-minute window as high-volume PDA or no PDA. The model was evaluated using 5-fold cross validation with stratification. Forward-stepwise feature selection was performed to reduce any overfitting.
Results: The model included a total of 80 TnECHOs (n= 30 high volume shunt, n= 50 no PDA) from 56 patients with a mean birth weight and gestational age of 634 ± 179 grams and 24.3 ± 1.2 weeks, respectively. With all predictor variables included, the model achieved a testing area under the curve (AUC) of 0.8630 (95% CI 0.8003, 0.9257). After feature selection, the model achieved a testing AUC of 0.8936 (95% CI 0.8557, 0.9316) with 9 out of 14 predictor variables.
Conclusion(s): Identification of a high-volume shunt from a hsPDA is possible with high accuracy using logistic regression modeling. Further work should focus on identification of moderate-volume shunts in this manner and correlation with clinical outcomes.
.png)
.jpg)
