Neonatology
Session: Neonatal GI Physiology & NEC 2: Enteral Nutrition and Growth
524 - An Impedance and temperature-Based Platform for Accurate Feeding Tube Placement in Neonates
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 524
Publication Number: 524.1935
Publication Number: 524.1935

Anoop Rao, MD, MS
Clinical Assistant Professor
Lucile Packard Children's Hospital Stanford
Palo Alto, California, United States
Presenting Author(s)
Background: Feeding tube (FT) placement is vital for neonates unable to feed orally. Ensuring correct tube position and identifying misplacements are key to prevent complications. While methods such as auscultation or x-rays are common, more accurate techniques with reduced risks are a vital unmet for these vulnerable infants.
Objective: To evaluate accuracy of a novel impedance and temperature-based platform designed to predict safe intragastric placement of feeding tubes in neonates.
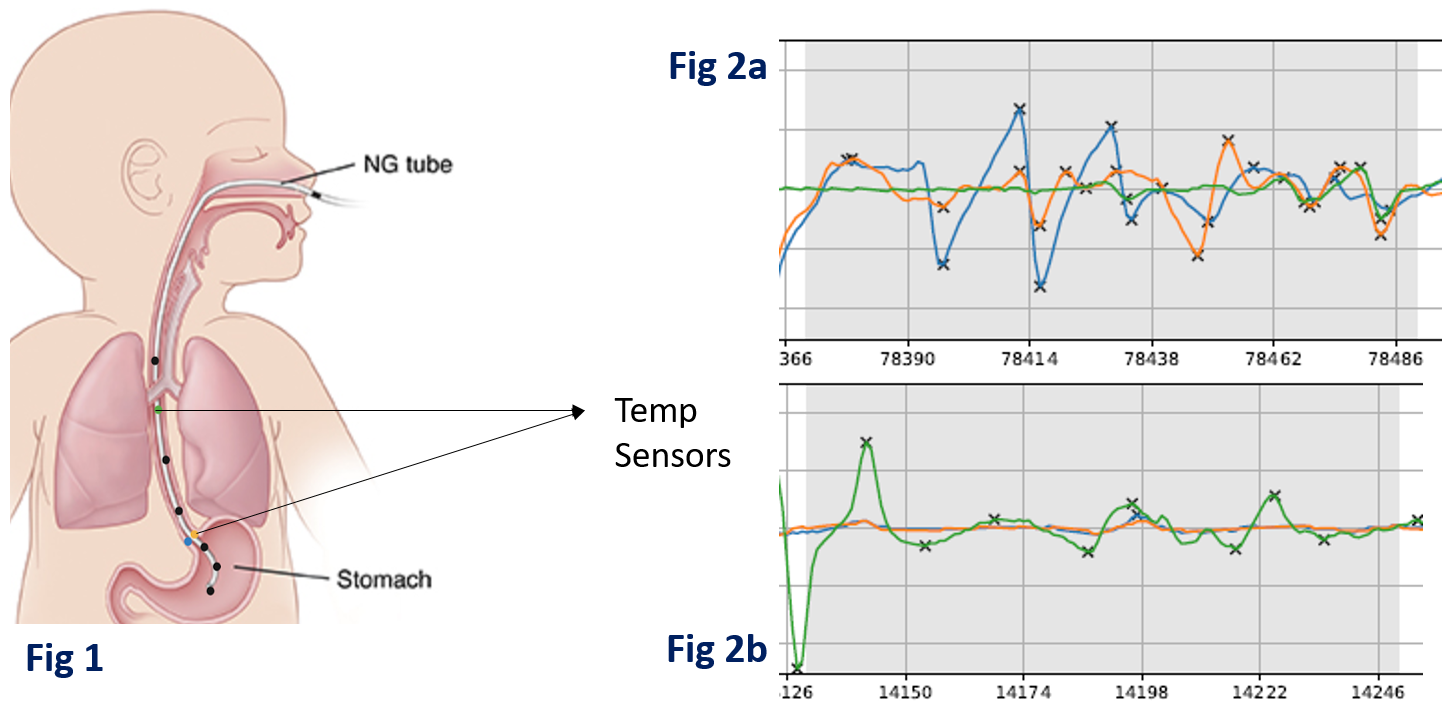
Design/Methods: The distal end of the 5 or 8Fr FTs were integrated with 6 electrodes and 3 temperature sensors (Fig. 1). During each placement attempt, the tube was inserted partially to a ‘safety check’ depth and paused for the temperature sensors to detect any fluctuations due to air flow. Temperature fluctuations, if detected, indicate that the tube is in the airway, not the esophagus. Notably, the clinical team was blinded to the results of the safety check and used standard methods for full insertion. Tube placement was eventually verified by auscultation, depth verification or X-ray per clinical team’s preference.
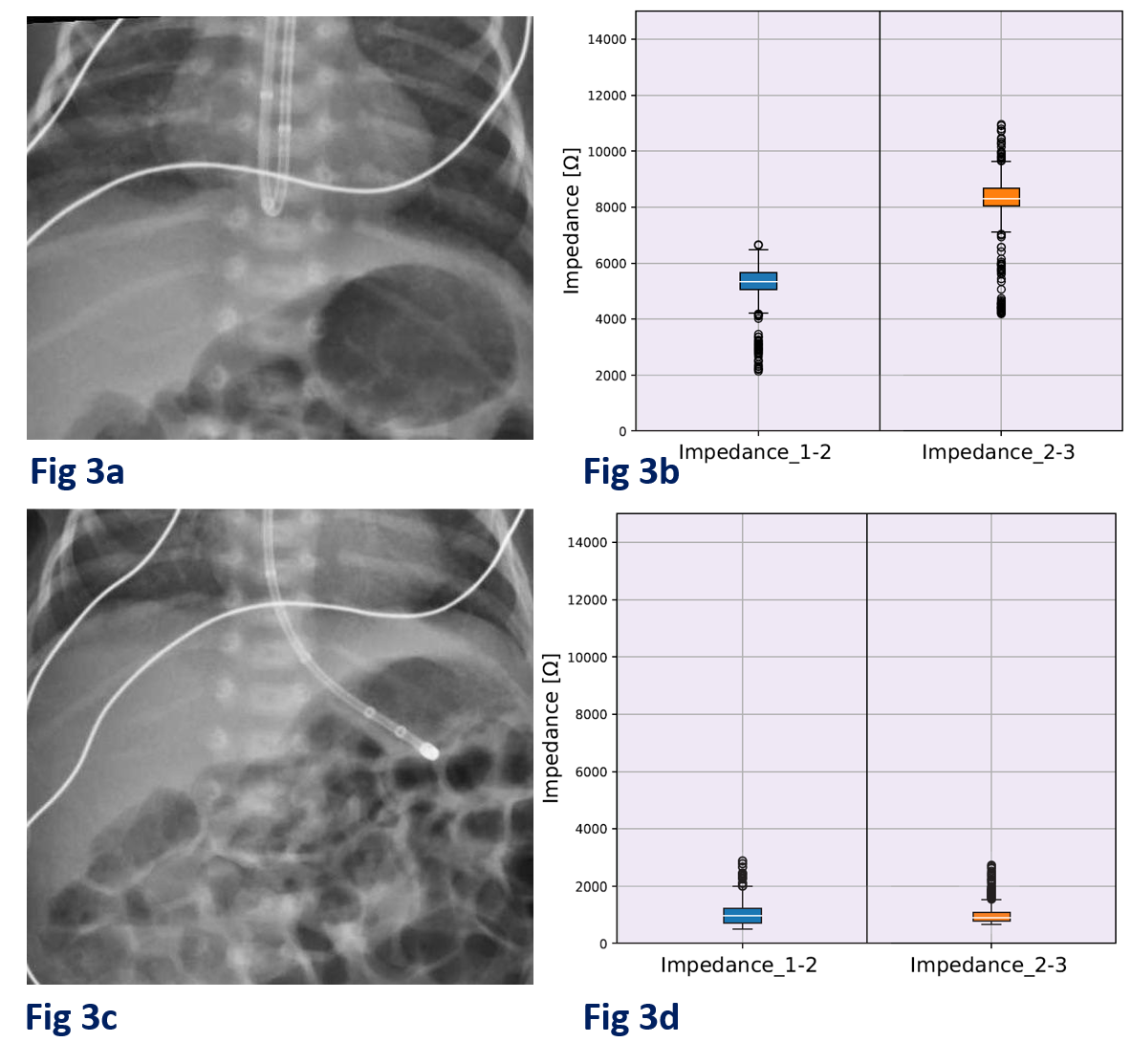
Results: In this IRB-approved study, 16 preterm neonates were enrolled. We made 20 feeding tube (FT) insertions using 5Fr (n=17) and 8Fr (n=3) tubes. Four needed a second attempt due to tubes curling into the esophagus or nasopharynx (n=2) or other placement issues (n=2). Of 6 X-rays, 5 confirmed gastric placement and one showed an esophageal kink (Fig. 2a).
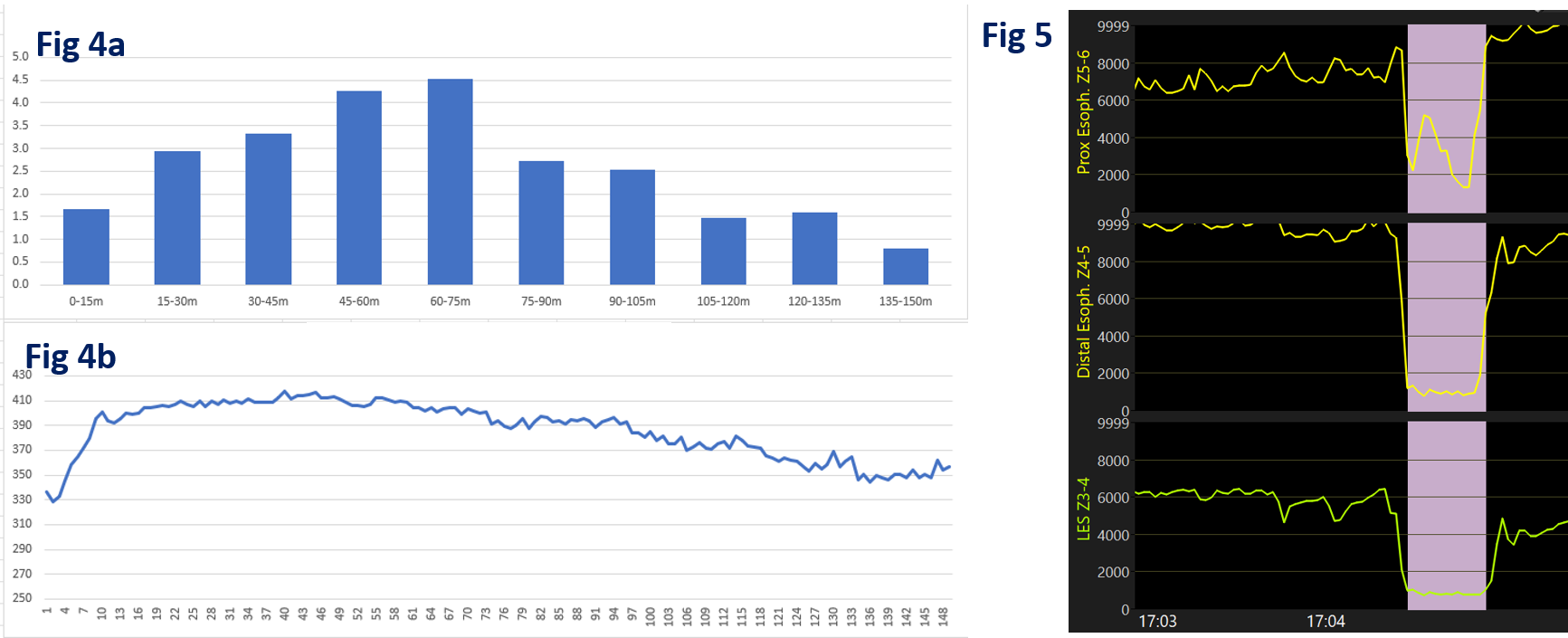
The temperature and impedance-based algorithm could accurately (a) identify location of FT as esophageal or airway (impedance > 2000Ω) and (b) identify intragastric positioning (impedance < 2000Ω) verified by abdominal x-rays. The algorithm integrates multiple physiologic parameters to determine the location of the feeding tube rather than solely relying on a fixed threshold. Additionally, the system can track (a) feeding and gastric emptying patterns by following the cyclical changes (4b) in impedance from low (~ 200Ω, in an empty, ionic fluid-rich stomach) to high (600-1000Ω, full stomach) and (b) reflux events (Fig 4a) because backwards flow of feeds lowers esophageal impedance (Fig. 5) momentarily.
Conclusion(s): In a novel neonatal study, we showed that our impedance and temperature-based method can accurately guide feeding tube placement, measure gastric emptying, and detect gastroesophageal reflux in real-time. The FDA has awarded the device a Breakthrough Designation based on these findings.