Neonatology
Session: Neonatal Pulmonology - Clinical Science 6: Respiratory/Neuro Outcomes, Steroids
584 - Racial/Ethnic Differences in Respiratory Medication Administration in Extremely Preterm Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 584
Publication Number: 584.3096
Publication Number: 584.3096

Stephanie R.R Diggs, MD (she/her/hers)
Instructor
Washington University St. Louis
Saint Louis, Missouri, United States
Presenting Author(s)
Background: Pulmonary complications, specifically the incidence of severe bronchopulmonary dysplasia (BPD) and development of pulmonary hypertension (pHTN), may differ by race/ethnicity among extremely preterm infants (EPT). It is unclear whether there are differences in respiratory medication administration by race/ethnicity.
Objective: To determine if there are differences in respiratory medication administration that may contribute to adverse respiratory outcomes among EPT Black or Hispanic infants.
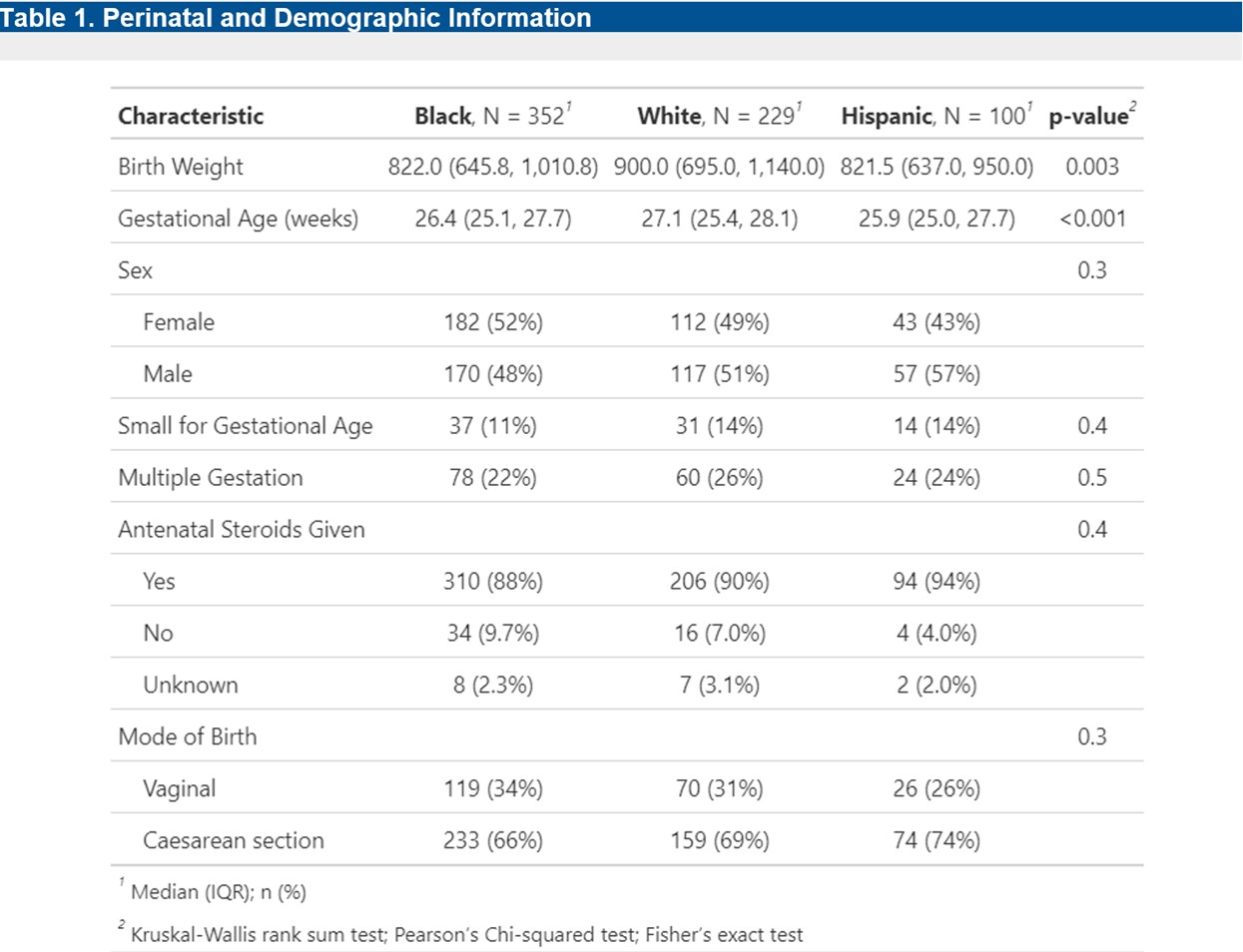
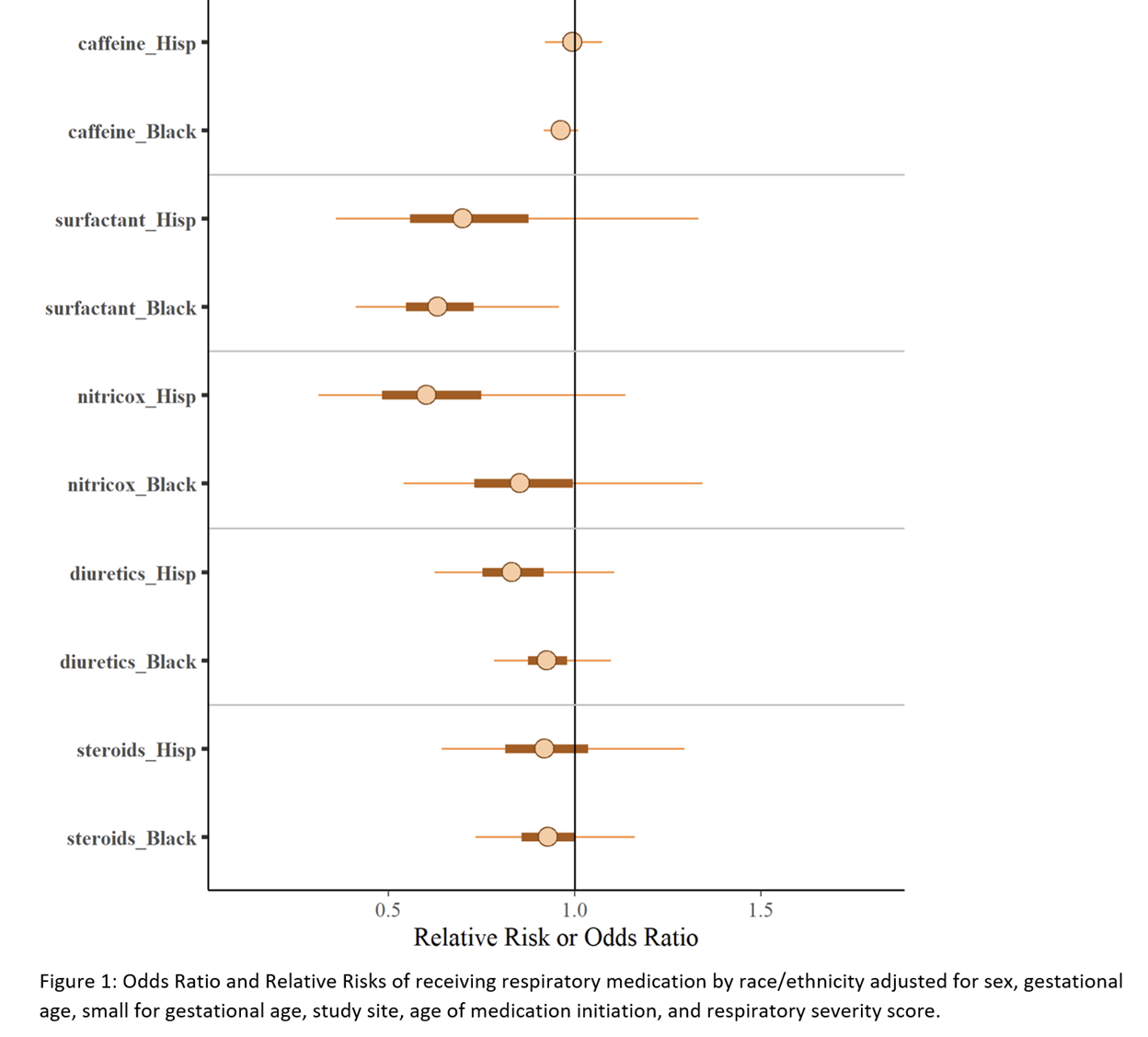
Design/Methods: We included infants 22-28 weeks’ gestation enrolled prospectively in the multicenter Prematurity-Related Ventilatory Control (Pre-Vent) observational study (NCT03174301). In this secondary analysis we evaluated non-Hispanic White, non-Hispanic Black, and Hispanic EPT infants based on maternal race/ethnicity. Use of respiratory medications (surfactant, caffeine, inhaled nitric oxide (iNO), diuretics [loop/thiazides], and postnatal steroids for BPD) were analyzed using Hurdle Poisson regression adjusted for sex, gestational age (GA), small for gestational age (SGA), center, mortality, and postnatal age and respiratory severity score (RSS, mean airway pressure x fraction of inspired oxygen) at medication initiation.
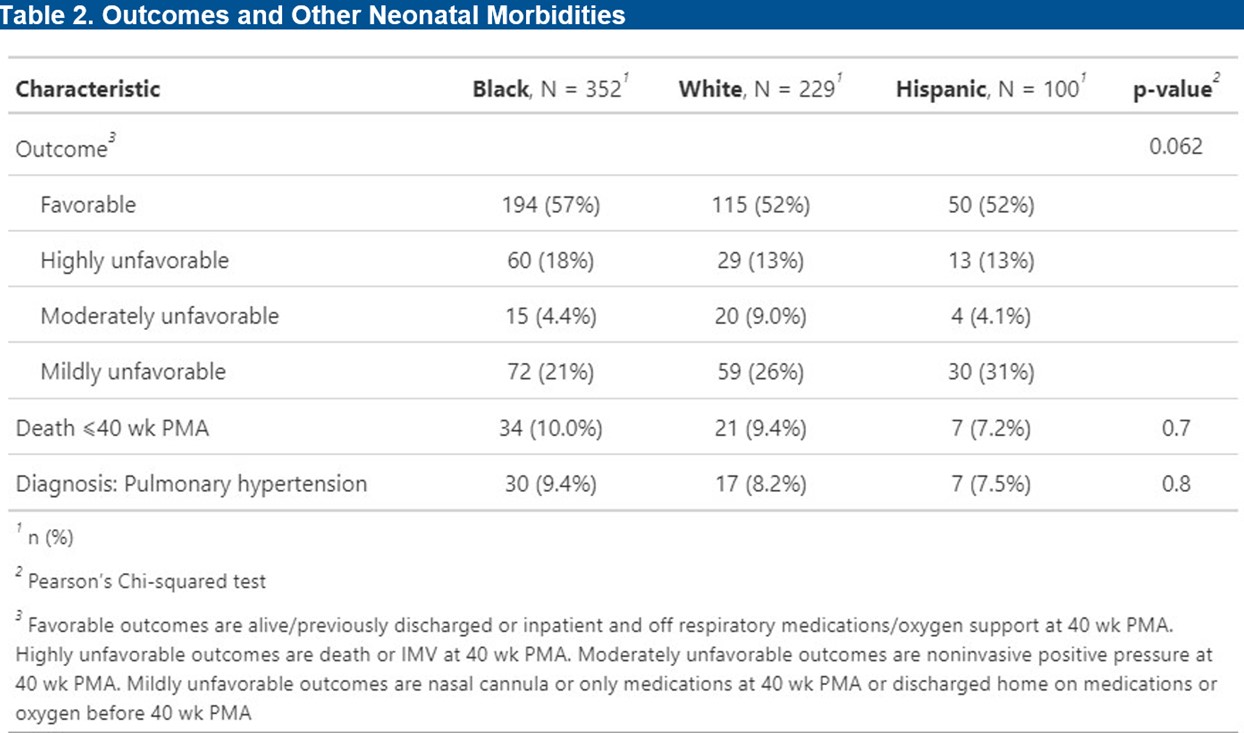
Results: We studied 681 EPT infants of whom 352 (51.7%) were Black, 229 (33.6%) were White, and 100 (14.7%) were Hispanic. The median GA and median birth weight (BW) differed by race/ethnicity (Table 1). In multivariable models, Black infants had lower odds of receiving surfactant compared with White infants (OR = 0.63 [95% CrI 0.41, 0.96]). The risk of receiving caffeine, iNO, diuretics, or postnatal steroids were not significantly different for Black or Hispanic infants compared with White infants (Figure 1). In a multivariable model, RSS was a statistically significant risk factor for receiving surfactant, iNO, steroids, and diuretics. However, there was no evidence of an interaction between RSS and medication use by race/ethnicity such that there were no difference in RSS between those who received or didn’t receive medications by race/ethnicity. In addition, there was no significant association between unfavorable respiratory outcomes, pulmonary hypertension, or death by race/ethnicity (Table 2).
Conclusion(s): Black EPT infants were less likely to receive surfactant compared with White infants, which may reflect differences in initial respiratory disease severity by race. There were no significant differences in use of other respiratory medications or differences in RSS at the time of medication initiation by race or ethnicity.