Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 3: Pulmonary Hypertension and Prematurity
111 - Association between Cardiovascular Care and Neurodevelopmental Outcomes in Infants with Neonatal Encephalopathy and Hemodynamic Instability
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 111
Publication Number: 111.1938
Publication Number: 111.1938

Kata Kovacs, MD, PhD (she/her/hers)
assistant lecturer; trainee in nonatology
Semmelweis University
Budapest, Pest, Hungary
Presenting Author(s)
Background: Patients with neonatal encephalopathy (NE) often present with hemodynamic instability during therapeutic hypothermia; however, thresholds for an approach to treatment of systemic low blood pressure is still not evidence based. We previously reported that approach to hemodynamic instability and patterns of brain injury are different between large centers, and showed that longer duration of cardiovascular medication is an independent risk factor for early adverse outcome.
Objective: Our primary aim was to analyze the approach to cardiovascular care and long-term outcomes in infants with NE at two high volume centers.
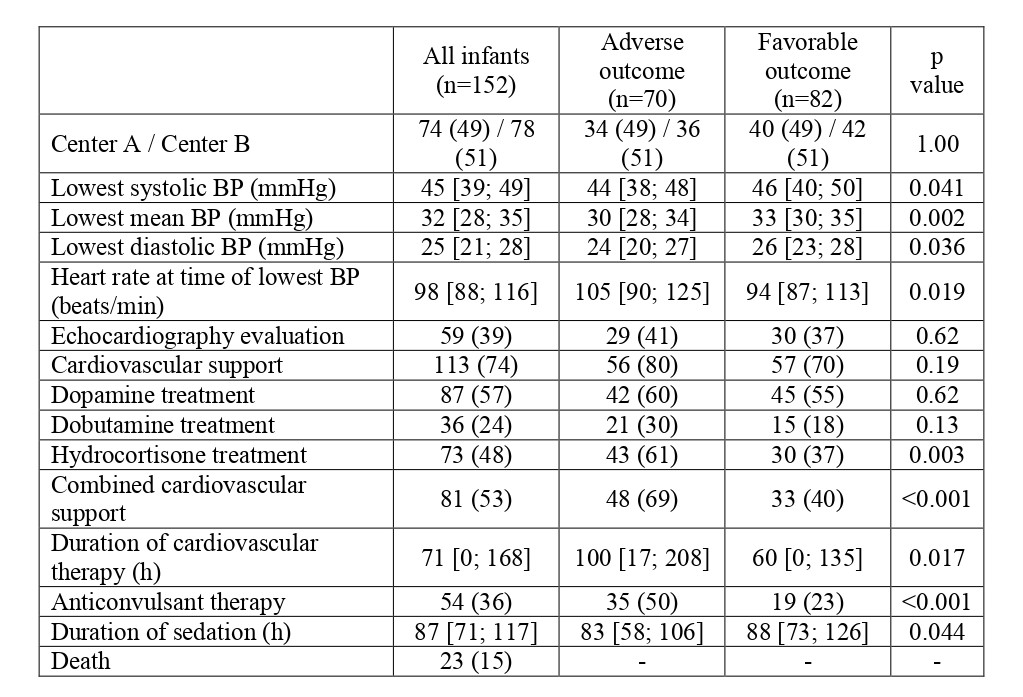
Design/Methods: In this retrospective cohort study, we studied 152 infants with moderate-severe NE, who (i) received therapeutic hypothermia in the NICU at the Hospital for Sick Children, Toronto, Canada (Center A, n=74) or the Pediatric Center, Semmelweis University, Budapest, Hungary (Center B, n=78) between 2015 and 2017, and (ii) developed systemic hypotension (mean arterial blood pressure < gestational age), and (iii) underwent neonatal follow-up. In Center A longitudinal targeted neonatal echo was often used to guide cardiovascular management, while Center B provided standard neonatal care. All infants had brain MRI examination in the first postnatal week and images were assessed according to the Barkovich scoring system. Neurodevelopmental follow-up was evaluated based on the Bayley-II and Bayley-III examinations and adverse outcome was defined as death or neurodevelopmental impairment ( < 70 points on Bayley-II or < 85 points on Bayley-III test).
Results: Rate of adverse composite outcome was similar in Center A and Center B (49% vs 51%, respectively) (Table 1). LASSO regression modelling revealed that the MRI results and the duration of cardiovascular treatment were associated with the primary outcome – assessed at median 19 [18; 21] month of age. The presence of hypoxic injury in the basal ganglia/thalamus and watershed area in the brain MRI increased the odds of adverse outcome by 10.5 fold (95% CI 4.58-26.0; p< 0.001), additionally for every 24 hours increase in the duration of cardiovascular support the odds of adverse outcome increased by 12% independent of the early MRI results (OR 1.12 95% CI 1.03-1.24; p=0.014). Although the approach to cardiovascular care and early MRI patterns differed between centers, site of neonatal care did not influence the long-term outcome.
Conclusion(s): Longer cardiovascular therapy was associated with an increased odds for adverse long-term outcome in patients with NE, independent of centers.