Neonatology
Session: Neonatal General 8: ROP, Neurology
306 - Beneficial effects of purine derivative drugs to treat severe hypoxic-ischemic brain injury in neonatal rats: Efficacy of intraperitoneal versus nose to brain drug delivery
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 306
Publication Number: 306.3122
Publication Number: 306.3122
- XC
Xiaodi Felix Chen, MD, PhD (he/him/his)
Associate Professor
Women & Infants Hospital of Rhode Island
Providence, Rhode Island, United States
Presenting Author(s)
Background: Hypoxic-ischemic encephalopathy (HIE) is a common neurological disorder that results in neurodevelopmental deficits such as cerebral palsy, behavioral and learning difficulties. Hypothermia is the only approved therapy. It provides partial protection and has limited efficacy in infants with severe HIE. Currently, there are no pharmacological treatments for HIE. Although we have shown that Purine Derivative Drugs (PDDs) attenuate moderate HI-related brain injury in neonatal rats, their efficacy in treating severe HI injury has not been examined. Moreover, we have previously given PDDs intraperitoneally (IP). Treatment by the IP route could limit the efficacy of the drug as because of first-pass hepatic metabolism. Nose-to-brain (N2B) drug delivery is a promising route to treat brain disorders and could represent a minimally invasive route for infants. Hence, equivalent doses of PPDs were given by the N2B and IP routes after exposure of neonatal rats to severe HI.
Objective: To determine (1) the neuroprotective efficacy of PDDs to treat severe HI-related brain injury and (2) whether IP or N2B drug delivery is more efficacious to treat severe HI in neonatal rats.
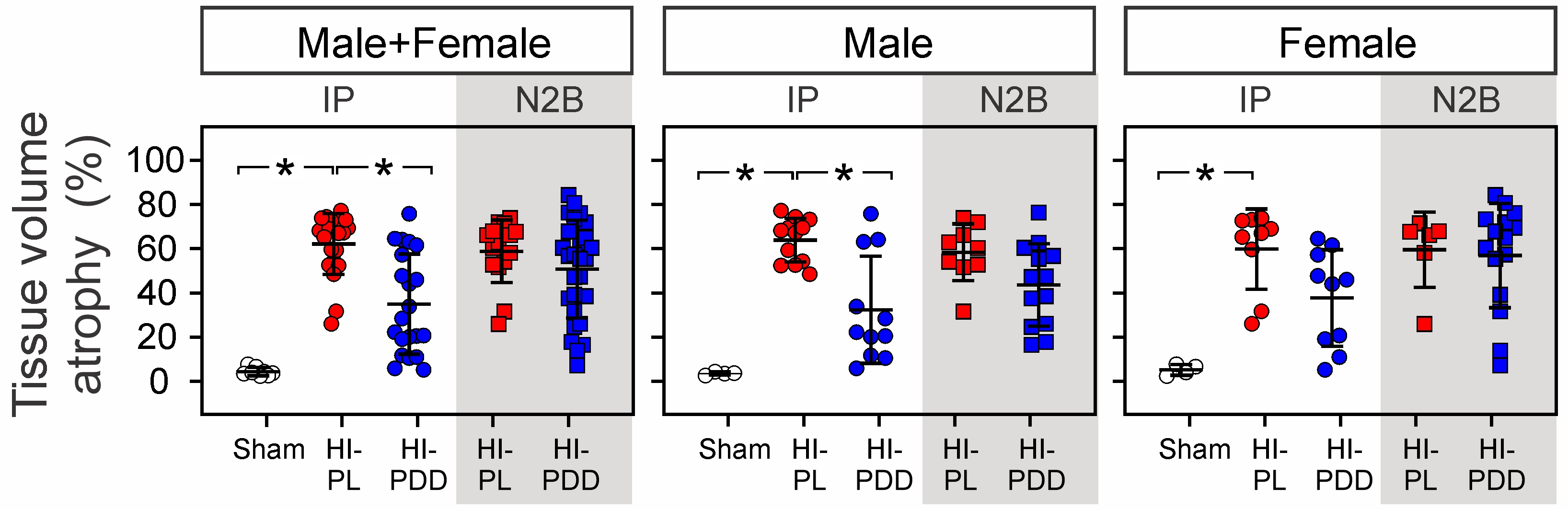
Design/Methods: Postnatal (P) day 7 rats were randomly assigned to 5 groups: Sham (IP), HI-placebo (HI-PL, IP), HI-PDD (IP), HI-PL (N2B), and HI-PDD (N2B) (Fig.). Rats were exposed to unilateral carotid artery ligation and 8% O2 for 120 min at 36°C. PL (phosphate buffered saline) or PDDs (30 mg/kg) were given IP or N2B at 0, 24, and 48 h after HI. 72 h after HI, brains were perfused and fixed. 20-μm coronal cryosections were stained with cresyl violet. Images of hemispheric tissue atrophy were analyzed with Image J (NIH). Infarct fraction was calculated as the percentage of the ratio of the damaged area to the area of the total hemisphere with correction for hemispheric swelling due to edema. Corresponding infarct volumes were calculated for the total set of slices.
Results: IP administration of PDDs significantly attenuated (P < 0.05, Fig.) hemispheric tissue volume loss in male+female and male neonatal rats exposed to severe HI-related brain injury. In contrast, N2B administration of PDDs did not reduce hemispheric tissue loss. However, statistical differences were not observed between HI-PDD (IP) and HI-PDD (N2B) groups.
Conclusion(s): PPDs exhibit neuroprotective effects in neonatal rats exposed to severe HI-related brain injury. However, the IP route but not the N2B route was more efficacious. Nevertheless, optimization including sample size and dosage considerations is required.