Asthma
Session: Asthma 2
198 - Health Equity and Unconscious Bias in Pediatric Asthma
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 198
Publication Number: 198.273
Publication Number: 198.273

Daniel Fein, MD
Associate Professor of Pediatrics
The Children's Hospital at Montefiore
teaneck, New Jersey, United States
Presenting Author(s)
Background: Unconscious and implicit bias by physicians has been shown to affect health outcomes in pediatrics. Racial and ethnic differences have been shown to exist in the management of pediatric asthma. We hypothesize that in addition to race, unconscious bias among physicians in regard to other social determinants of health (SDOH) may also affect treatment decisions and outcomes of pediatric asthma patients.
Objective: To identify unconscious and implicit biases in the management and treatment of pediatric asthma patients by comparing differences between stated and derived importance of demographic, social and clinical factors for treatment decisions.
Design/Methods: A web-based survey was disseminated to a variety of providers of pediatric asthma care. The survey contained questions about demographics, perceptions of health equity and eight auto-generated patient profiles. There were 5832 possible patient profiles with the following variables: gender, age, race, exposure to environmental triggers, annual household income, prior treatment, current symptoms and level of rescue medication used. Figure 1 displays a sample patient profile.
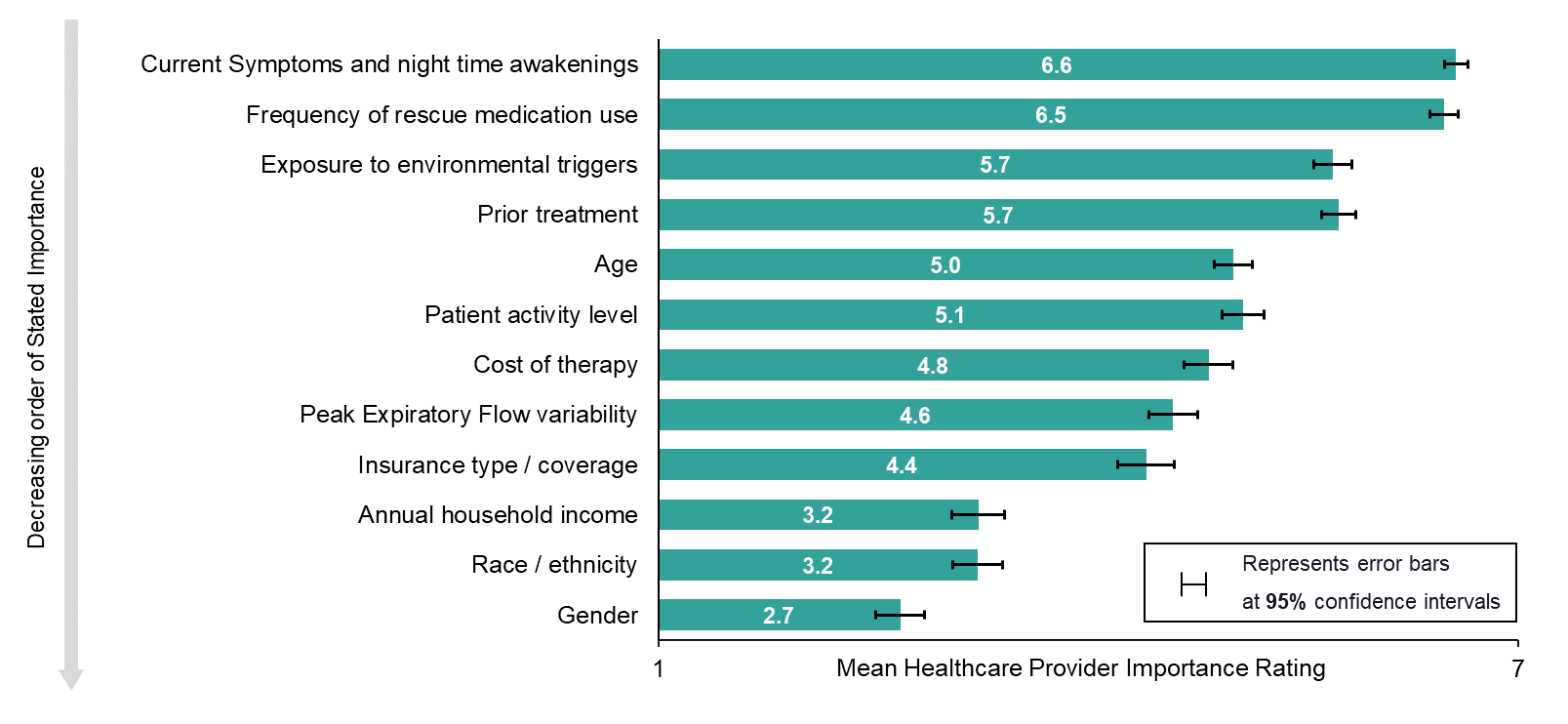
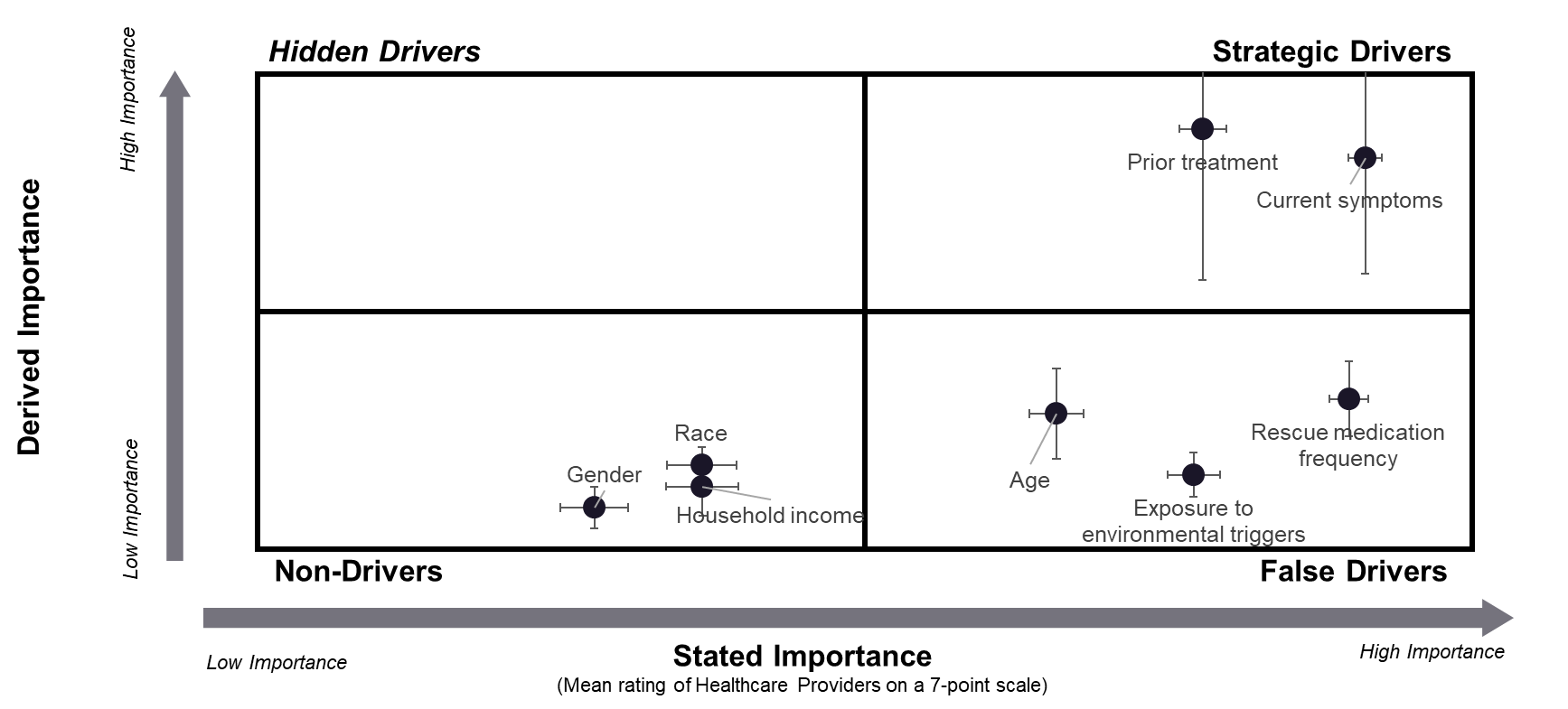
Results: 307 physicians completed the survey, the majority of whom were community-based physicians (235 (77%)) between the ages of 35-54 (184 (60%)). One-hundred and seventeen (38%) of respondents were familiar with health equity with 120 (39%) stating their organization currently or previously had a program involving SDOH and/or health equity and 129 (42%) agreeing that systemic racism leads to unfair treatment of certain groups. Clinical factors had a higher importance than non-clinical factors when making treatment decisions (Fig 2). Race, gender and household income were both stated and derived as low importance factors in making treatment decisions while prior treatment and current symptoms were both stated and derived as high importance factors. Age, rescue medication frequency and exposure to environmental triggers were stated as high importance factors but derived as low importance (Fig 3).
Conclusion(s): Most physicians surveyed were not familiar with health equity. Prior treatment and current symptoms were the clinical factors that factored most into clinician decisions for asthma treatment. Demographic and social factors contributed less to physician decision making.