Neonatology
Session: Neonatal General 2: NICU Care Strategies
66 - A Large Neonatal Network Nutritional Consensus for High Risk Neonates
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 66
Publication Number: 66.211
Publication Number: 66.211
.jpg)
Sarvin Ghavam, MD (she/her/hers)
Attending Physician, Director of Clinical Practice Guidelines and Standards
Childrens Hospital of Philadelphia
Moorestown, New Jersey, United States
Presenting Author(s)
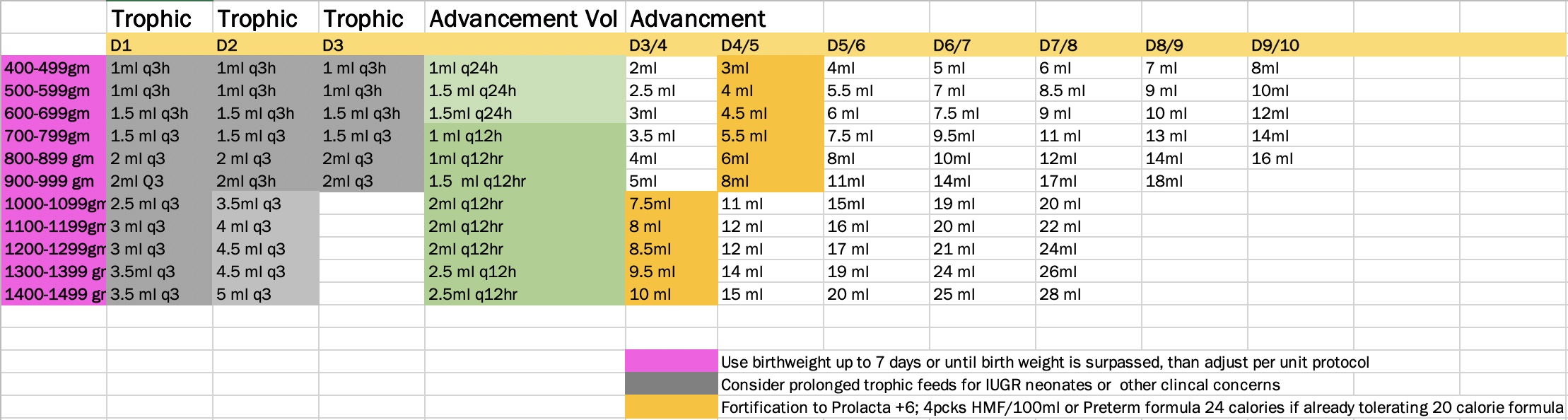
Background: Nutrition provided to premature neonates impacts weight gain, linear growth, neurodevelopment, chronic lung disease, sepsis and NEC. Standardization of feeding protocols has shown to decrease the incidence of NEC. Research supports early feeding advances up to 30ml/kg/day do not increase the rates of NEC and improve time to full enteral feeds with decreased length of TPN. Rapid enteral advance also decreases extrauterine growth restriction and improves short term outcomes. Earlier fortification improves protein intake without deleterious effects, with positive impact on chronic conditions and long-term growth.
Objective: Evaluate pre and post implementation data following an evidence-based consensus project among a 14 Newborn Network hospitals seeking consistency in feeding practices for neonates born < 32 weeks and < 1500 gm birthweight. Objectives included providing optimal feed advancement and fortification and without impacting necrotizing enterocolitis (NEC) rates
Design/Methods: After rigorous review of the literature, a consensus statement was created to standardize parenteral and enteral nutrition for high risk infants within a large neonatal network in late 2020. Following implementation, data was collected 6-12 months prior to and 1-2 years post implementation among the 4 largest in-born units by retrospective chart review.
Outcomes assessed included: NEC, central line days, % fortification at 60ml/kg/day, days on TPN, age feeds started and delta z score from birth to discharge or 36 weeks. Data collected include: gestational age, birth weight, sex, and content of first feed.
Results: A total of 359 patients were analyzed, 121 patients pre-implementation and 238 post implementation. For CVL and TPN days, patients who died, those with early transfer to OSH or incomplete data were excluded. Age starting feeds and central line days were all significantly reduced (Figure 2); fortification at 60ml/kg/day significantly increased. There was no significant change in the incidence of NEC or change in mortality. Although not significant, the delta z-score change from birthweight to discharge or 36 weeks shows a trend towards improvement.
Conclusion(s): A unified evidence-based approach across multiple large level III NICUs with a multi-disciplinary team showed significant benefit in nutritional support for high risk neonates and proved that consistency in care is possible in large neonatal networks.
.png)
.png)