Neonatology
Session: Neonatal Pulmonology - Clinical Science 2: Lung Imaging, Lung Function
202 - The Association between Initial Chest X-ray, Early Respiratory Support and Mortality or Bronchopulmonary Dysplasia in Very-Low-Birth-Weight Preterm Infants Using Machine Learning
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 202
Publication Number: 202.3134
Publication Number: 202.3134

Tsung-Yu Wu (he/him/his)
Attending physician
Ditmanson Medical Foundation Chia-Yi Christian Hospital
TAINAN CITY, Tainan, Taiwan (Republic of China)
Presenting Author(s)
Background: Early identification of high-risk infants with bronchopulmonary dysplasia (BPD) is essential for clinical decision-making. According to Jensen's new definition of BPD, the relationship between early oxygen therapy, ventilator support, the initial chest X-ray (CXR), and the BPD diagnosis remains uncertain.
Objective: Our study aimed to investigate the impact of these respiratory characteristics within the first two weeks of life on the diagnosis of BPD using a machine learning (ML) approach.
Design/Methods: This single-center retrospective cohort study enrolled neonates admitted to our NICU with a birth weight (BW) of < 1500g and a gestational age (GA) of < 32 weeks between January 2017 and December 2020.
Within the first two weeks of life, we collected hourly accumulated FiO2 (aFiO2), accumulated mean airway pressure (aMAP), and accumulated respiratory severity score (aRSS) for each neonate. In addition, the initial CXR obtained on the first day of life was analyzed using image embedding with transfer learning of deep neural networks as an additional variable.
Neonatal risk factors included GA, BW, gender, mode of delivery, Apgar scores at 1 and 5 minutes, and the presence of RDS requiring surfactant. Relevant variables were identified using the rank widget's scores.
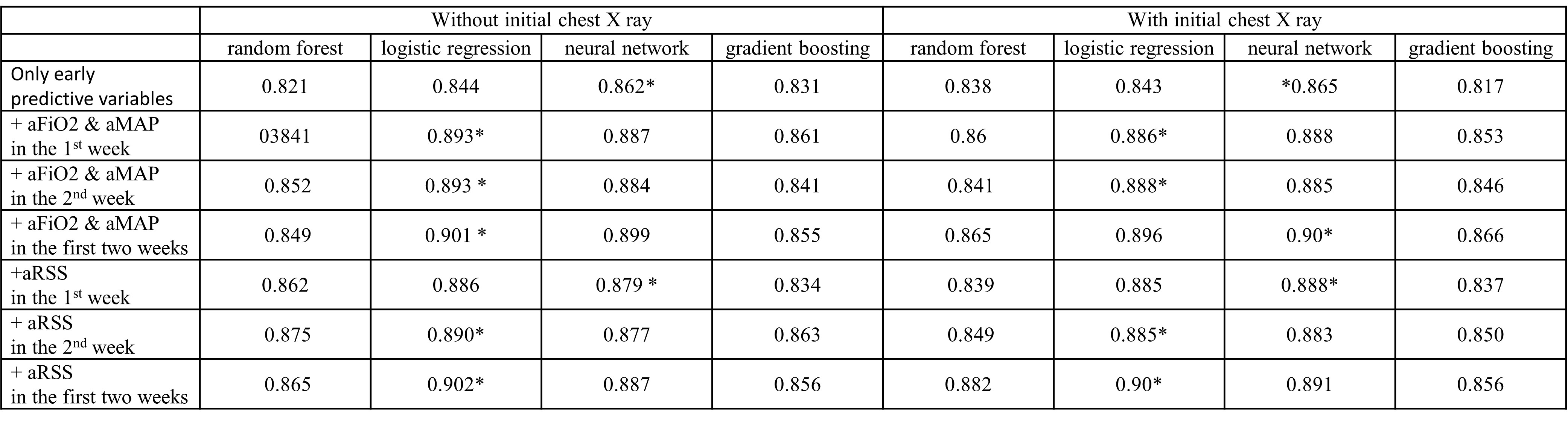
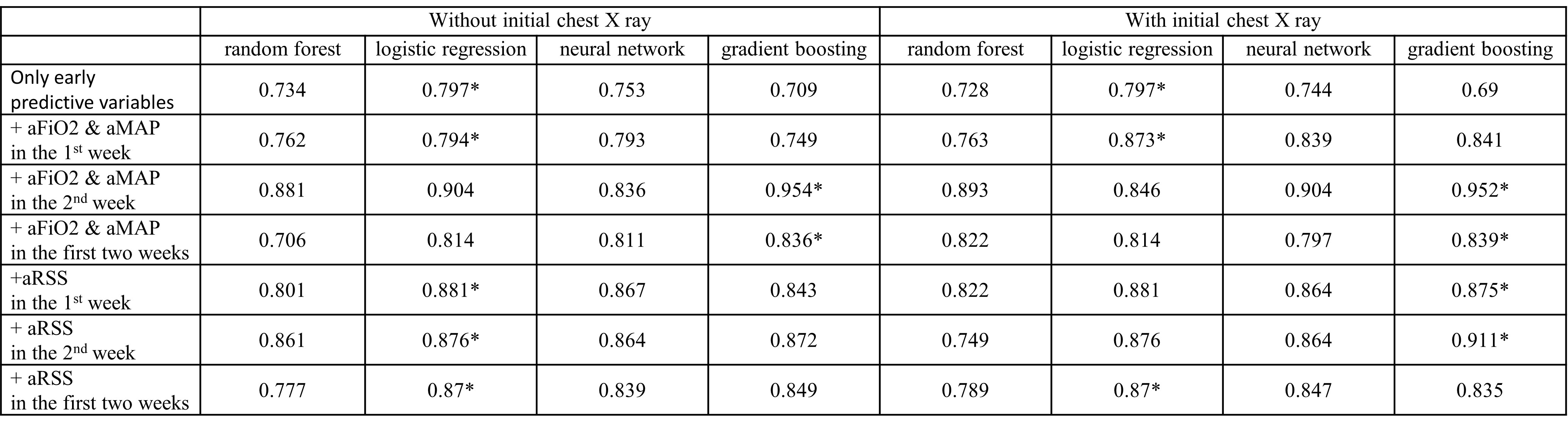
ML models using multiple algorithms were used to identify risk factors associated with mortality after 2 weeks of life and the diagnosis of BPD based on the initial CXR, as well as the aFiO2, aMAP, and aRSS within varying postnatal periods (the first week, the second week, and the first 2 weeks).
Results: We enrolled 250 neonates (2.4% BPD in grade I, 44.0% in grade II, 4.0% in grade III, 48.4% without BPD, and 1.2% undetermined due to death before diagnosis). For predicting mortality or BPD, the aFiO2, aMAP, and aRSS over different postnatal periods exhibited excellent discriminatory ability (area under the receiver operating characteristic curve [AUC]: 0.794-0.902). In the second week, aFiO2 and aMAP had the highest AUC (0.954) for mortality. The aRSS within the first two weeks had the highest AUC (0.902) for the diagnosis of BPD. However, initial CXR did not enhance the diagnostic efficacy of the predictive models for BPD.
Conclusion(s): We effectively implemented CXR into predictive models by combining image embedding with transfer learning. Initial CXR evaluation did not substantially enhance our predictive abilities. In the first two weeks of life, based on aFiO2, aMAP, and aRSS, we could predict mortality or BPD.
.jpg)
