Mental Health
Session: Mental Health 1
552 - Strengths and Well-Being Assessment: Positive Psychiatry in Primary Care for Adolescents with Mental Health and Substance Use Concerns.
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 552
Publication Number: 552.1804
Publication Number: 552.1804

Valerie S. Harder, PhD, MHS (she/her/hers)
Associate Professor
Robert Larner, M.D., College of Medicine at the University of Vermont
Burlington, Vermont, United States
Presenting Author(s)
Background: As the pandemic highlighted gaps in meeting adolescent behavioral health (mental health and substance use) needs, primary care practitioners (PCPs) were a locus for interventions to address adolescent behavioral health. Strengths-based approaches may support PCP promotion of positive behavioral health in adolescents, but competing priorities or other factors may inhibit their use for all patients universally.
Objective: The main objective of this study was to assess utilization of strengths-based approaches during the health supervision visit (HSV) for adolescents with and without behavioral health concerns.
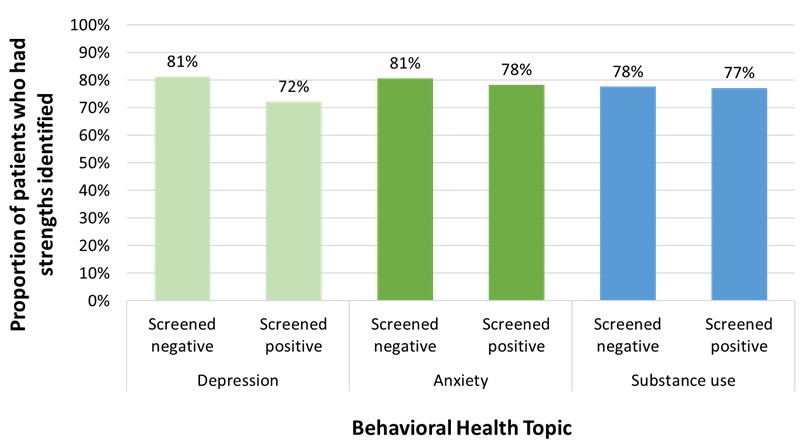
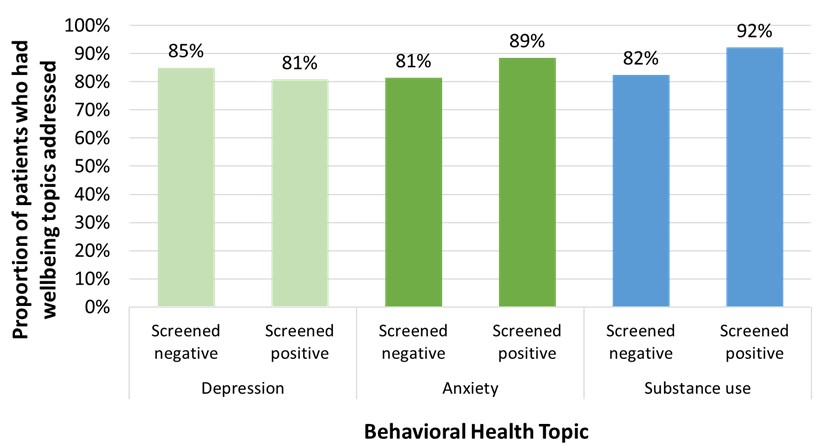
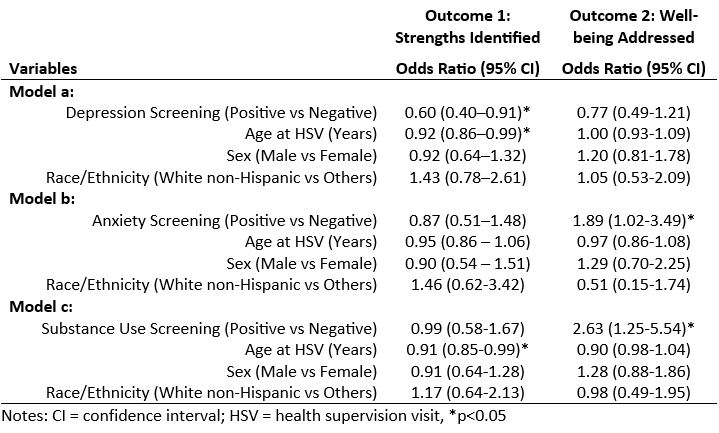
Design/Methods: Using randomly sampled health record data from 31 primary care practices across Vermont, the study population included 1,494 adolescents 12-21 years old. We examined two strengths-based approach outcomes, 1) strengths identified (e.g., generosity) and 2) well-being topics addressed (e.g., exercise) and three screening variables, 1) depression, 2) anxiety, and 3) substance use. We compared strengths-based approach utilization between those with positive behavioral health screening results and those without, using multiple logistic regression models, controlling for the potential confounding effects of age, sex, and race/ethnicity, using p< 0.05.
Results: Among the 986 patients seen for an HSV, 78% had strengths identified and 83% had well-being topics addressed during the visit, while 89% were screened for depression, 43% for anxiety, and 88% for substance use. Multiple logistic regression analyses revealed that adolescents screening positive for depression were 40% less likely to have had strengths identified than those screening negative (p=0.016), and no associations between having strengths identified and anxiety or substance use screening (ps>0.60). Results for well-being revealed no association with depression screening (p=0.25); however, adolescents screening positive for anxiety were 89% more likely to have had well-being addressed than those screening negative (p=0.042), and adolescents screening positive for substance use were 163% more likely to have had well-being addressed than those screening negative (p=0.011).
Conclusion(s): As PCPs are asked to do more within HSVs, they may need support for integrating strength-based approaches when managing adolescents screening positive for depression.